With its ability to accurately detect more malignant prostate cancer lesions than transrectal ultrasound (TRUS)-guided biopsy, multiparametric MRI can reduce the frequency of the invasive procedures by as much as 28%, according to a multicenter, international study presented at last week's European Association of Urology Congress in Copenhagen.
The findings come from the Prostate Evaluation for Clinically Important Disease: Sampling Using Image Guidance or Not? (PRECISION) trial, which also were published online on 19 March in the New England Journal of Medicine. By opting first for a noninvasive MRI scan rather than biopsy, researchers believe the modality could greatly change the approach to prostate cancer.
"PRECISION shows that using an MRI to identify suspected cancer in the prostate and performing a prostate biopsy targeted to the MRI information leads to more cancers being diagnosed than the standard way that we have been performing prostate biopsy for the last 25 years," said lead author Dr. Veeru Kasivisvanathan from the University College London in the U.K.
Biopsy risks
Prostate cancer is the most common cancer among men, with some 400,000 new cases every year in Europe. In the U.K. alone, there are more than 46,000 new cases of prostate cancer every year, leading to more than 11,000 deaths. In the U.S., the American Cancer Society estimates there will be approximately 164,000 prostate cancer cases and some 29,000 deaths in 2018.
Currently, TRUS-guided biopsy is the most common method to diagnose cases of suspected prostate cancer. The procedure involves invasively taking samples from a patient using a probe with a needle under local anesthetic. Along with a slight risk of infection, the biopsy also is unreliable because clinicians must estimate the location and position of a lesion and abnormalities are often missed.
"This study was the first to allow men to avoid a biopsy," added study co-author Prof. Mark Emberton of University College London, senior investigator with the National Institute for Health Research. "If high-quality MRI can be achieved across Europe, then over a quarter of the 1 million men who currently undergo a biopsy could safely avoid it."
For this study, researchers from 23 centers in 11 countries randomly enrolled 500 men between February 2016 and August 2017 for either a standard 10 to 12 core TRUS biopsy or an initial 1.5-tesla or 3-tesla MRI scan. A follow-up targeted biopsy was performed if the MR images showed evidence of an abnormality. Of those subjects, 252 participants were assigned to the MRI-targeted biopsy group, while the remaining 248 men were in the standard-biopsy group.
Clinically significant prostate cancer was defined as a Gleason Grade of 3+4, while clinically insignificant cancer was deemed Gleason Grade of 3+3. In addition, MRI results were graded on the PI-RADS version 2 scale of 1 to 5, with 1 as no cancer and 5 as highly likely to be prostate cancer. Patients with a score of 3, 4, or 5 underwent MRI-targeted biopsy.
Within the MRI-targeted biopsy group, 71 subjects (28%) did not undergo biopsy because their MRI scans did not suggest prostate cancer. Of the subjects with a positive cancer result on multiparametric MRI, 51 men (29%) had a PI-RADS version 2 score of 3; 70 patients (40%) had a score of 4; and 54 (31%) participants had a score of 5.
Head-to-head
In the direct comparison between the two cancer evaluation methods, MRI-targeted biopsy was statistically superior to biopsy by confirming 95 men (38%) with clinically significant cancer, compared with 64 confirmed cases (26%) in the standard-biopsy group (p = 0.005).
In addition, MRI-targeted biopsy reported statistically significant fewer patients with a diagnosis of clinically insignificant cancer (23 men, 9%), compared with standard biopsy (55 men, 22%) (p < 0.001).
"We also found that patients who had MRI had fewer side effects than those who just had the standard TRUS biopsy," said Kasivisvanathan, who presented the results at the conference. "This is because the MRI allows some men to avoid biopsy and in those who need one, is able to better indicate which area of the prostate needs to be investigated so you don't need to randomly sample the whole prostate and can use fewer biopsy cores."
While the results are certainly encouraging, the authors noted the need for appropriate training for clinicians to use MRI and biopsy, and for healthcare service providers to increase the availability and capacity to perform prostate MRI.
"The ability to perform good quality MRI and the ability to interpret the MRI information are specialist skills," Kasivisvanathan added. "In the long term, this new diagnostic pathway can be cost-effective. Costs can be saved by the reduction in the number of men undergoing biopsy in the first place, by the earlier diagnosis of harmful cancers and in the avoidance of the diagnosis of harmless cancers."
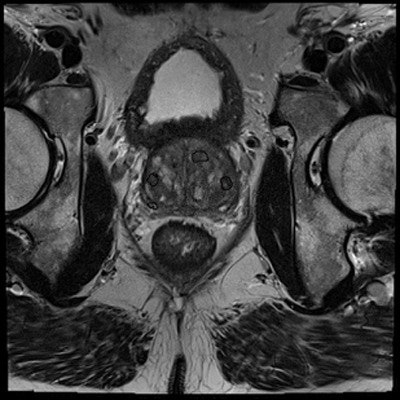
Editor's note: Image on the home page courtesy of Geert Litjens, Radboud University Medical Center in Nijmegen, the Netherlands.