Both PET/MRI and PET/CT perform admirably in the initial staging of breast cancer patients, but there are subtle nuances between the hybrid modalities of which clinicians should be aware, according to a Swiss study presented earlier this month at ECR 2018 in Vienna.
Researchers' per-lesion analysis found that PET/MRI achieved greater sensitivity, while PET/CT was significantly better with specificity. The key differentiator comes down to the bone.
"PET/MRI had superior sensitivity than PET/CT in the per-lesion assessment, mainly due to bone metastases," said Dr. Diomidis Botsikas from the department of radiology at Geneva University Hospitals. "But there was no significant difference [between the modalities] in the per-patient analysis, and diagnostic confidence with both examinations was similar."
Modality preferences
Initial staging for breast cancer is critical for patients so they can receive the most appropriate treatment as soon as possible to increase their chances for survival. For almost two decades, PET/CT has been the modality of choice for this clinical application, but researchers also have seen the benefits of PET/MRI to evaluate different stages of breast cancer.
"We know that whole-body PET/CT is recognized as one of the best techniques for staging of advanced disease," he told ECR attendees. "We wanted to see if whole-body PET/MRI combined with dedicated breast MRI would have better locoregional and distant staging ... of initial staging of breast cancer."
The Swiss researchers prospectively recruited 80 consecutive patients (mean age of 55.3 years, ± 7.7 years) who underwent a PET/MRI scan and PET/CT scan for initial staging of breast cancer between August 2010 and July 2016.
Two readers with experience in both hybrid-imaging modalities evaluated the datasets and recorded all suspicious lesions in the contralateral breast, auxiliary lymph nodes, internal mammary lymph nodes, mediastinal lymph nodes, and other potentially metastatic sites.
There was at least a two-month interval between reading sessions. A percutaneous biopsy and/or pathology report was used as the standard of reference. If neither source were available, the researchers used a patient's follow-up evaluation at least 12 months later.
Direct comparisons
The researchers calculated sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) for both modalities, along with the correlation of PET/MRI and PET/CT for lymph node (N) and metastatic (M) staging based on the reference standards. In addition, the diagnostic confidence for both modalities on each lesion was noted.
Overall, the researchers discovered 101 metastatic lesions in 51 (64%) of the 80 subjects. Interreader agreement on the results was rated as excellent for PET/CT (0.833) and PET/MRI (0.823).
The per-lesion analysis revealed a statistically significant difference between PET/MRI and PET/CT in sensitivity, but PET/CT performed better than PET/MRI for specificity.
| Per-lesion analysis | |||
| PET/MRI | PET/CT | P value | |
| Sensitivity | 89% | 77% | 0.0013* |
| Specificity | 96% | 98% | 0.0075* |
| Positive predictive value | 82% | 89% | |
| Negative predictive value | 98% | 96% | |
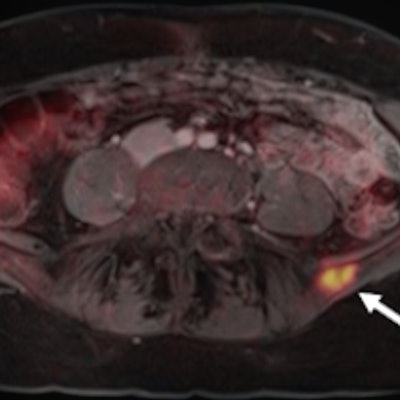
The statistically significant difference between the two hybrid modalities in sensitivity and specificity was due primarily to their performance relative to the 26 (51%) bone lesions found in nine patients (11%).
| Bone-lesion analysis | |||
| PET/MRI | PET/CT | P value | |
| Sensitivity | 92% | 69% | 0.0034* |
| Specificity | 95% | 100% | 0.0081* |
| Positive predictive value | 77% | 100% | |
| Negative predictive value | 99% | 95% | |
The differences between PET/MRI and PET/CT were not statistically significant in the evaluation of other tumors. For example, 48 axillary lymph nodes were found among 46 patients (57%), with the two modalities achieving similar performances for sensitivity and specificity.
| Axillary lymph node analysis | |||
| PET/MRI | PET/CT | P value | |
| Sensitivity | 85% | 81% | 0.157** |
| Specificity | 89% | 92% | 0.257** |
| Positive predictive value | 77% | 81% | |
| Negative predictive value | 93% | 92% | |
There were 10 internal mammary lymph nodes discovered among nine patients (11%). The two modalities achieved identical sensitivity (90%), specificity (100%), PPV (100%), and NPV (99%). The results also were the same between PET/MRI and PET/CT for six mediastinal lymph nodes found in six patients (7%). Both modalities scored 100% for sensitivity, specificity, PPV, and NPV.
For four contralateral breast lesions in three patients (4%), PET/MRI was better than PET/CT for sensitivity (100% versus 33%, respectively) and positive predictive value (75% versus 50%, respectively). However, there were too few samples to definitively determine statistical significance.
On the per-patient analysis, there were 13 M-1 patients with distant metastases in bone, the liver, pulmonary, mediastinal, and/or thoracic wall. PET/MRI achieved sensitivity of 85% for these patients, compared with sensitivity of 69% for PET/CT. There was, however, no statistically significant difference between the modalities (p = 0.157). There also was no statistically significant difference between the two modalities for specificity, PPV, and NPV in M-staging.
Similarly, for N-staging of lymph nodes in the per-patient analysis, there were no statistically significant differences between the two modalities for all lesions, axiallary or lymph nodes, internal mammary lymph nodes, metastatic lymph nodes, and contralateral breast lesions.
| Initial breast cancer staging | ||
| PET/MRI | PET/CT | |
| N-staging | 0.484 | 0.536 |
| M-staging | 0.917 | 0.800 |
"In conclusion, diagnostic confidence with both examinations was similar," Botsikas said. "PET/MRI had superior sensitivity mainly for bone metastases than PET/CT in the per-lesion assessment, but there was no significant difference in the per-patient analysis."
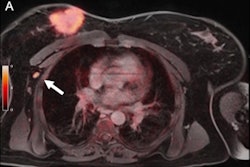
Editor's note: The image used to introduce this article on our home page is a PET/MRI image of a patient with recurrent breast cancer and a PET-positive bone metastasis of the left iliac wing. Image courtesy of Dr. Johannes Grueneisen at Essen University Hospital in Germany.