Clinicians can use CT angiography (CTA) or digital subtraction angiography (DSA) scans to construct customized 3D-printed models of brain vessel abnormalities that replicate real-life cases, according to a study published in the British Journal of Neurosurgery.
In the pilot study, researchers from China formatted the CTA and DSA scans of two patients with a brain arteriovenous malformation (AVM) to create 3D-printed vascular models. They found that measurements of the vascular models were very similar to the dimensions of their corresponding scans, with less than 10% deviation (Br J Neurosurg, 15 January 2018).
What's more, showing the patient-specific 3D-printed brain AVM models to patients and surgical residents improved patient-to-physician communication as well as enhanced resident training, according to the authors led by Dr. Guangzhong Chen from Guangdong General Hospital.
"An actual physical model ... offers a stereoscopic sense, the viewer can touch the object and actively move it with hands, which can offer more sensory process than just viewing the images controlled with mouse operation, and surgeons can develop a deeper understanding of the anatomy and can easily acquire knowledge when dealing with blood vessels," they wrote.
High fidelity
Numerous groups have created 3D-printed models based on CT scans or MR images and applied them to patient education as well as surgical planning and training. Physicians working on complex cases have recently begun testing the viability of using other modalities to build these models instead of relying on CT and MRI alone.
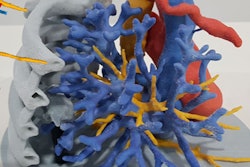
Tasked with treating two patients who had an intricate vessel deformation in the brain, Chen and colleagues performed a CTA on one patient and a DSA on the other for visualization. They observed that one patient had an irregular tangle of arteries and veins around the left middle cerebral artery, and that the other had a similar malformation by the right posterior cerebral artery.
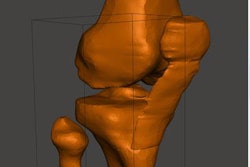
To get a more intuitive look at the vasculature, the researchers used computer software (Mimics 14, Materialise) to process the scans and form a 3D fusion image of the skull bone and blood vessels. They converted these files into stereolithography format, loaded them into a different software (Magics 9.51, Materialise) for further 3D reconstruction, and finally produced the models with a 3D printer (J750, Stratasys).
Both of the 3D-printed brain AVM models demonstrated high fidelity compared with their originating scans, the authors wrote. A comparative analysis showed there was a 97% agreement in measurements of blood vessel diameter and less than 10% deviation.
Neurosurgeons presented the 3D-printed model based on CTA scans to the first patient in order to explain to him about his condition and the surgical procedure they planned on performing. The patient gave the educational experience a maximum positive score of "5" on a scale of overall satisfaction, and the neurosurgeons described the model as "very useful" for engaging the patient in discussion.
The team used the second 3D-printed model, based on DSA scans, to help train surgical residents at the hospital. Among 20 residents, 16 reported the 3D-printed brain AVM model improved their spatial understanding of the brain AVM more than simply viewing DSA scans did, and 18 residents considered the model to be a helpful educational tool.
Visually meaningful
The 3D-printed brain AVM models are useful for visualizing and understanding key aspects of the condition such as the location of the AVM nidus, its position relative to feeding arteries and draining veins, and areas that could be affected by rupture of the AVM, according to the authors. This is particularly relevant for patients and young surgeons.
"CTA or DSA [scans] are important for the doctor but meaningless visually to the patients," they wrote. "Preoperatively printed patient-specific 3D models can be used to improve patient communication and to enhance trainee's ability to compare 2D imaging with a tangible 3D reality."
However, incorporating the 3D-printed model into patient education and surgical training might not be practical just yet due to its high price. Each model costs approximately $700 (564 euros) to make, and the entire process of image reconstruction and 3D printing can take more than 20 hours to complete.
Overcoming this barrier is the next step on the group's agenda, along with creating life-size models of brain vasculature that would allow for an in vitro assessment of vessel hemodynamics. Currently, the vessel walls of the 3D-printed brain AVM models have different physical properties from human vessels, which prevents users from effectively evaluating the lumen and wall of the vessels.
"In the future, with the development of medical imaging technology and 3D-printing technique, we can reconstruct brain AVM models mimicking the vascular structures and its mechanical properties," they wrote. "As 3D printing technology evolves and its cost reduces, patient-specific 3D-printed brain AVM models may become routine for both clinical and educational use."