Researchers are reporting early success in the combination of optical and molecular imaging to view FDG-PET images that detect early-stage breast cancer. The technique, known as Cerenkov luminescence imaging (CLI), can assess tumor margins during breast tumor surgery by detecting light emitted from an FDG-PET radiopharmaceutical.
If validated clinically, CLI could become the first option rather than breast-conserving surgery, which is currently the most widely chosen initial treatment, according to Dr. Arnie Purushotham, chair of breast cancer and professor at King's College London, and colleagues (Journal of Nuclear Medicine, June 2017, Vol. 58:6, pp. 891-898).
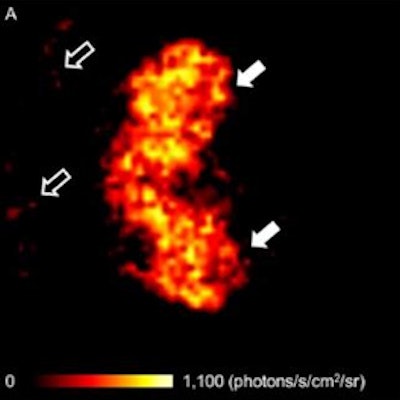
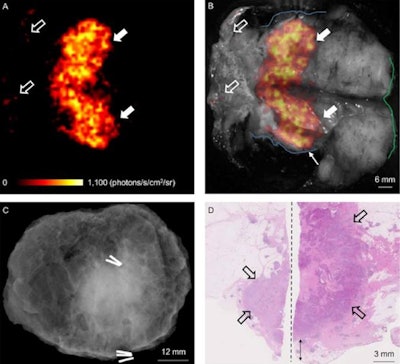 Image set comes from a patient with grade 3, ER-/HER2-, no special type carcinoma and includes the Cerenkov image (A) and a grayscale photographic image (B) overlaid with Cerenkov signal. An increased signal from the tumor is visible (white arrows). Both surgeons measured the posterior margin (outlined in blue) as 2 mm (small arrow) and the medial margin (outlined in green), which measured more than 5 mm. A phosphorescent signal also is visible (open arrows), along with specimen radiography image (C). The absence of one surgical clip to mark the anterior margin, and the odd position of the superior margin clip (white arrow) prevented reliable margin assessment. A combined histopathology image (D) from two adjacent pathology slides on which the posterior margin (bottom of image) and part of the primary tumor are visible (open arrows). The distance from the posterior margin measured 3 mm microscopically (double arrow). Images courtesy of the Journal of Nuclear Medicine.
Image set comes from a patient with grade 3, ER-/HER2-, no special type carcinoma and includes the Cerenkov image (A) and a grayscale photographic image (B) overlaid with Cerenkov signal. An increased signal from the tumor is visible (white arrows). Both surgeons measured the posterior margin (outlined in blue) as 2 mm (small arrow) and the medial margin (outlined in green), which measured more than 5 mm. A phosphorescent signal also is visible (open arrows), along with specimen radiography image (C). The absence of one surgical clip to mark the anterior margin, and the odd position of the superior margin clip (white arrow) prevented reliable margin assessment. A combined histopathology image (D) from two adjacent pathology slides on which the posterior margin (bottom of image) and part of the primary tumor are visible (open arrows). The distance from the posterior margin measured 3 mm microscopically (double arrow). Images courtesy of the Journal of Nuclear Medicine.Approximately one in five women who undergo lumpectomy require repeat surgery due to inadequate excision of the tumor during the initial surgical procedure, but by accurately assessing tumor resection margins intraoperatively with CLI, surgeons may be able to completely clear the cancer with a single operation so that breast cancer patients undergo fewer follow-up surgical procedures, the researchers explained. Ultimately, CLI could enhance patient care and reduce healthcare costs, if confirmed in larger clinical studies.
In the JNM study, Purushotham and colleagues enrolled 22 patients with invasive breast cancer. The imaging protocol included injection of FDG 45 to 60 minutes prior to surgery. Immediately after the excision of tumors, they imaged specimens intraoperatively with an investigational CLI imaging system.
The group used the first 10 patients to optimize the imaging protocol while the other 12 patients were included in the analysis dataset. Ten of the 12 patients had an elevated tumor radiance on CLI, with good agreement between researchers who rated margin distance. Sentinel lymph nodes also were successfully detected and biopsied in all patients with the help of a technetium-99m radiopharmaceutical.
The researchers suggested that intraoperative CLI may become a feasible imaging technique in combination with FDG-PET across a range of solid cancers, and provide adequate clinical evaluation in other solid cancer types that also experience incomplete tumor resection.