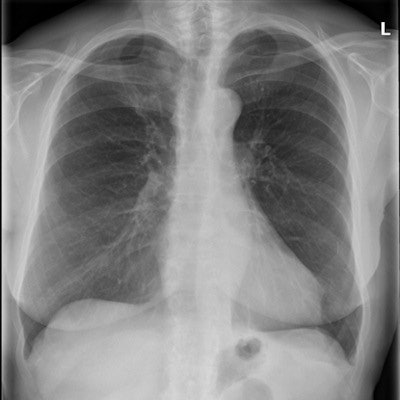
In the quest to diagnose mild-stage chronic obstructive pulmonary disease (COPD), radiologists often use chest radiographs, but Dutch researchers of a new study advise that they shouldn't do so because it results in substantial overdiagnosis.
The researchers performed a retrospective, nested case-control study of patients who underwent both spirometry and chest radiography to compare the diagnostic accuracy of the latter. They compared only a subset of the controls from the cohort to the incident cases. The team, led by Dr. Annemarie den Harder, a radiologist and doctoral candidate at the University Medical Center Utrecht in the Netherlands, found chest radiographs resulted in a sensitivity of 10% (European Journal of Radiology, 9 May 2017).

"This study has raised the awareness at our institution that it is very challenging to diagnose COPD based on a chest radiograph," she wrote in an email to AuntMinnieEurope.com. "Therefore, we discourage our colleagues and general radiologists to mention suspicion of COPD in chest radiograph reports. We did not quantify the influence on reporting, but from our experience we think that COPD is mentioned less often in the reports after this study."
Why chest x-ray?
Chronic obstructive pulmonary disease is usually diagnosed and classified by spirometry. However, in patients with respiratory symptoms, a chest radiograph is generally the first test performed, and, thus, radiologists often mention COPD, frequently as an incidental finding.
"The largest challenge is that chest radiographs are made very often for a large variety of indications," den Harder noted. "In our hospital, around 20% of all radiological examinations are a chest radiograph."
Could that use rate of routine, preoperative chest radiographs translate into detecting mild COPD without overdiagnosis? That's precisely what the researchers sought to determine.
Their study included 783 patients referred for cardiothoracic surgery who routinely received preoperative chest radiographs and spirometry on the same day. However, they included only patients with stage I and II COPD, leaving 155 cases.
The researchers defined COPD using the Global Initiative for Chronic Obstructive Lung Disease (GOLD) classification system. They used a digital flat-panel detector system with a tube potential of 125 kV and determined the mAs value using automated exposure control. Both a posteroanterior (PA) and a lateral chest radiograph were acquired for each patient.
Two senior radiology residents and one board-certified chest radiologist with more than 10 years of experience in thoracic radiology assessed for COPD signs on the radiographs. Observers were blinded for COPD status and did not have access to clinical information. To assess interobserver variability, each of the three observers scored 30 randomly selected patients. All observers scored overall appearance of the chest radiographs specific for COPD.
The implications
The researchers found 20% (155/783) of the patients had mild-stage COPD. For the board-certified radiologist, the positive predictive value (PPV) for overall appearance of the chest radiograph specific for COPD was 55%, negative predictive value (NPV) was 84%, sensitivity was 27%, and specificity was 95%. Only 26% (41/155) of the COPD cases were detected, while a similar proportion of 22% (34/155) of the patients without COPD were wrongly classified as having COPD.
"In routine clinical practice, we think it is important in diagnosing COPD as an incidental finding to reach a high PPV to prevent substantial overdiagnosis," the authors wrote. "This can be achieved when only patients with a predicted probability of 0.97 or higher are classified as having COPD."
Doing so would result in a PPV of 100%, NPV of 82%, sensitivity of 10%, and a specificity of 100%, making it possible to detect 10% of patients with mild COPD without any false positives.
"However, as soon as more COPD patients are detected by also classifying patients with a lower predicted probability as having COPD, this results in a disproportionally large increase in the number of false positives because the PPV rapidly declines with smaller predicted probabilities," they added.
It's clear from the results that performance of chest radiography for diagnosing mild COPD is limited.
"Based on the findings of this study, specialists and general practitioners should be aware of the limited diagnostic value of chest radiographs for COPD," the authors wrote. "This should be discussed with patients to prevent unnecessary anxiety, and confirmation with spirometry should be obtained when COPD is mentioned in chest radiography reports."
Better still, don't mention suspicion of COPD in chest radiography reports at all: "It is possible to detect COPD patients in some extent; however, this will result in substantial overdiagnosis, which is associated with a waste of resources on unnecessary care," they added.
Den Harder and colleagues are performing several other studies on COPD imaging, but using CT instead of conventional imaging, including a large multicenter study that investigates the use of a chest CT instead of a conventional chest radiograph prior to cardiac surgery (the CRICKET study).



















