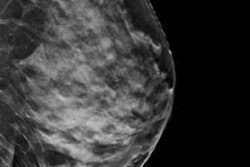
Digital breast tomosynthesis (DBT) identifies more breast cancers than conventional digital mammography, according to two studies presented at ECR 2017. In addition, the recall rates between the two modalities are comparable, researchers found.
Both studies examined the use of DBT in a screening setting. In one, the researchers found DBT identified 80% more cancers than digital mammography. In the other, the researchers found the rate of screen-detected breast cancer was about 50% higher for women screened with DBT compared with women screened with digital mammography.
In an era in which the question continues to be whether DBT is ready to replace digital mammography for breast cancer screening, evidence keeps mounting in DBT's favor.
Italian study
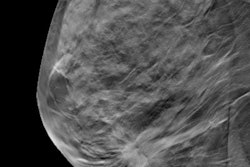
In the first study, researchers from the northern Italian city of Reggio Emilia analyzed data from more than 19,000 women who were randomized to receive either digital mammography or digital mammography plus DBT from March 2014 to March 2016. Each patient had a double screening examination only once, according to researcher Dr. Valentina Lotti from Arcispedale Santa Maria Nuova in Reggio Emilia.
 Dr. Valentina Lotti.
Dr. Valentina Lotti.Consenting women ages 45 to 70 years old were randomized into either study arm. The digital mammography arm included 9,782 women, while the DBT plus mammography arm included 9,623 women.
Digital mammography detected 45 cancers (six in situ) and digital mammography plus DBT detected 79 cancers (14 in situ).
The overall relative detection rate was 1.8, while the relative detection rate for in situ cancer was 2.4. The researchers found no difference by breast density. However, DBT showed major improvement for smaller tumors (10 mm to 20 mm) as the relative detection rate was 2.6.
"In our randomized trial, 80% more cancers were identified in the study arm compared with the control arm. This detection is similar for in situ, invasive, pT1 [small] cancers, and dense and fatty breasts," Lotti said.
Norwegian study
 Dr. Tone Hovda.
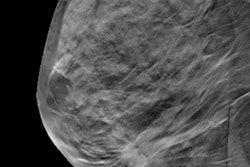
Dr. Tone Hovda.In the next study, Dr. Tone Hovda and colleagues from Drammen Hospital in Drammen, Norway, compared the recall rate and rate of screen-detected breast cancer after one year of screening with synthetic images and DBT versus digital mammography in the Norwegian Breast Cancer Screening program. They found that the screen-detected cancer rate increased by 50% in the DBT arm.
A total of 18,172 women ages 50 to 69 residing in Oslo were screened with DBT (Hologic) in 2014, while a control group of 30,883 women were screened with digital mammography (Siemens Healthineers, GE Healthcare, and Hologic).
The control group was chosen because it had comparable recall rates and cancer detection rates to Oslo (the study arm) in the prestudy period, but all the women were located in the same region of Norway.
| Comparison of DBT vs. digital mammography | ||
| Digital mammography | DBT | |
| Recall rate | 32.6 per 1,000 (3.3%) | 31.7 per 1,000 (3.2%) |
| Invasive cancers detected | 5.5 per 1,000 | 7.2 per 1,000 |
| Ductal carcinoma in situ | 0.9 per 1,000 | 2.1 per 1,000 |
| Positive predictive value (PPV) of recalls | 19.9% | 29.2% |
| PPV for biopsy at recall | 40% | 55.3% |
The findings indicate that the recall rate did not differ for DBT versus digital mammography, most probably due to an already low recall rate in Norway. In addition, DBT providers had previous experience with tomosynthesis screening because of the earlier Oslo tomosynthesis screening trial in the study group, Hovda said.
However, the PPV of recalls and biopsy were higher for the experimental group than for the control group.
"This implies the number of false-positive recalls is reduced for the tomosynthesis group, and this is an important benefit both to women and society as it reduces the burden of unnecessary recalls," she said.
Because of the increased rate of screen-detected breast cancer of nearly 50% for those screened with synthetic 2D and DBT compared with those screened with regular 2D digital mammography, and reduction of false positives, DBT is the superior modality, she noted.
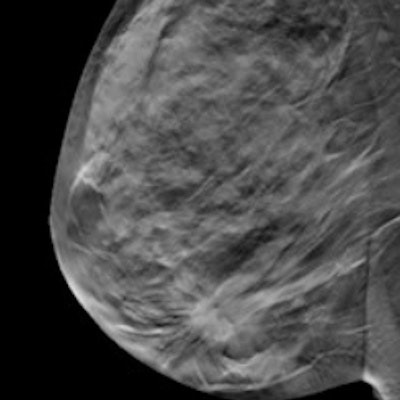
Concerns over the added radiation dose of DBT due to the need for a 2D acquisition have been addressed through the use of synthesized 2D mammography, in which the 2D image is derived from DBT data.
Other objections to DBT as a screening tool include increased reading time, increased data load, issues of overdiagnosis, and what type of extra cancers will be diagnosed. All of these issues need further investigation, she concluded.