Researchers from a top London teaching hospital with extensive experience of infectious diseases have shared their knowledge of performing imaging examinations on patients with the Ebola virus and given practical recommendations on how to minimize problems in future epidemics.
The World Health Organization (WHO) declared the end of the Ebola outbreak in Sierra Leone in March 2016, and in Guinea and Liberia in June 2016, but the departmental protocol developed at the Royal Free Hospital in London remains applicable to any subsequent highly contagious patients admitted to the high-level isolation unit (HLIU), according to Dr. J.E. Bretherton, consultant radiologist Dr. Dylan Tsukagoshi, and colleagues.
 Around 28,000 cases of Ebola were reported in Guinea, Sierra Leone, and Liberia in 2015 and 2016. There were more than 11,000 deaths in these countries alone.
Around 28,000 cases of Ebola were reported in Guinea, Sierra Leone, and Liberia in 2015 and 2016. There were more than 11,000 deaths in these countries alone."All [Ebola] patients required chest radiographs for confirmation of tube and line positioning, and some patients required further imaging to assess for complications of the illness/treatment such as pulmonary edema," they reported in an e-poster presentation at RSNA 2016. "A small number of radiographs were of suboptimal quality as patients had to position the cassette themselves, but images were obtained without issue and all were of adequate quality to answer the clinical question posed."
At the Royal Free, a large protective sleeve component of the isolation tent is used for the x-ray tube head. The x-ray cassette is inserted into a similar sleeve, and if conscious, the patient can position the cassette; otherwise, it is placed under or behind the bed. No radiographic equipment passes into the isolation tent or comes into direct contact with the patient.
For highly contagious patients, all requests for imaging must be made on a consultant-to-consultant basis, ideally between 9 a.m. and 5 p.m., the researchers noted. Medical doctors in the third year of training or above should perform the ultrasound scans, and all staff must change into surgical scrubs. In the Royal Free, radiographers wear personal protective equipment, and HLIU staff members assist with the cleaning and changing into and out of the equipment. X-rays are interpreted in the department using the hospital PACS, a dedicated portable ultrasound machine remains onsite, and patients no longer considered infectious are imaged with standard infection-control precautions.
Developing crisis
Ebola virus disease (EVD) was first recorded in 1976 in two simultaneous outbreaks in Nzara, Sudan (now South Sudan), and Yambuku, Zaire (now the Democratic Republic of Congo). The latter outbreak occurred near the Ebola river, the authors explained. Subsequent outbreaks (< 500 cases) occurred in West Africa over the next three decades, and the start of the world's largest and most complex outbreak came in 2014. WHO reported more than 28,000 cases in Guinea, Sierra Leone, and Liberia in 2015 and 2016, with over 11,000 deaths, and further cases occurred in Nigeria and Senegal.
The disease, formerly known as Ebola hemorrhagic fever, is a severe and often fatal viral illness, and the average case fatality rate is around 50%. The virus is believed to be a zoonosis occurring in primates; fruit bats are thought to be the natural reservoir host, Bretherton and colleagues stated.
Symptoms occur between two and 21 days following infection and include fever, headache, myalgia, fatigue, diarrhea and vomiting, abdominal pain, and unexplained bleeding and bruising. This can progress to severe thrombocytopenia and hemorrhage, abnormal liver function, multiorgan failure, and death. There is currently no licensed treatment for the disease, although experimental treatments have been used. Management is predominantly supportive.
"The role of imaging in EVD is limited and primarily supportive," noted the authors, adding that imaging is used to assess complications and exclude alternative pathology. Importantly, it is used for central venous catheter insertion and position confirmation of tubes and lines.
The Royal Free approach
The high-level isolation unit was set up in 2008. The scope of imaging is confined to portable ultrasound and x-ray exams. The unit occupies an entire ward of the hospital and is always fully prepared for an admission, according to the authors. Previous admissions include a patient with Crimean Congo hemorrhagic fever admitted in 2012 who died in the hospital. Half of the floor space is occupied by a negative pressure air filtration and recirculation system, which excludes all particles, including viruses. There are two specialized isolation tents with an adjacent overflow unit with capacity for six patients.
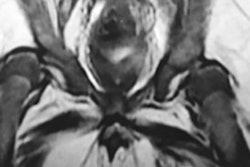
In the unit, the patient is contained within an isolation tent under negative pressure ventilation, and medical staff do not enter the isolation tent. Items can be passed into the tent via the access tunnel. Blind-ending side sleeves allow medical staff to insert their arms to examine the patient, move items within the isolation tent, and perform certain procedures. Imaging equipment also can be operated in this way.
Three repatriated patients with confirmed EVD and one with and unconfirmed case (later tested negative) have been admitted to the Royal Free. All three patients with confirmed disease were successfully treated and discharged, the researchers explained. No healthcare workers became infected, but one patient was later readmitted with complications.
"The first patient was repatriated at relatively short notice, therefore an official departmental protocol for imaging had not yet been devised at the time of their admission. There was some uncertainty among clinicians and radiology department workers regarding scope of imaging and how safety of staff would be ensured," they pointed out.
Shortly before the first patient's arrival, the departmental portable ultrasound was taken to the unit for a trial run, but the machine did not fit into the bed space, so an older portable ultrasound machine for vascular access was placed in the isolation unit. The scanner had to be disposed of after the patient was discharged as the sterilization regime, involving hydrogen peroxide, was too destructive.
The team had to source a new ultrasound unit, either with disposable probes to use within the isolation tent, or a machine that could be operated entirely outside the tent to remove the need for sterilization. They chose a Siemens Healthineers Acuson Freestyle machine, because the probe is cable-free and images are wirelessly transmitted to the screen in real-time.
"To scan, the operator inserts the probe into a designated side sleeve in the isolation tent. Additional medical staff can use further side sleeves to expose the area for scanning and apply the ultrasound gel (if the patient is unable to do this themselves). The machine is kept permanently in the isolation unit. Similarly to our departmental portable ultrasound machine, there is currently no link to PACS," Bretherton and colleagues wrote.
The departmental protocol includes plans for increased numbers. If more than two patients are admitted, the third and additional patients would be nursed in the adjacent overflow unit. The overflow unit is a modified conventional ward, and it does not have isolation tents or a negative pressure air filtration system, so protective suits would be required. Imaging would not be possible in these patients, unless a dedicated portable x-ray machine was purchased and disposed of afterward, they continued.
"Overall, as expected, there was minimal requirement for imaging in this patient group," they concluded. "Chest radiographs were the single most requested and performed imaging investigation. There was no requirement for ultrasound; some requests were discussed, but these were deemed invalid, i.e., result would not change patient management."