New Swiss research shows that adding computer-aided detection (CAD) in ultralow dose CT significantly improves sensitivity for detecting solid pulmonary nodules. This may be a crucial step in the early detection of lung cancer and lead to better patient outcomes, according to the study authors, who pointed to a reported relative survival rate for non-small cell lung cancer of 80% without recurrence when detected at a local stage.
The study appeared online in the European Journal of Radiology (11 October 2016) and is due for publication in the December 2016 issue. It shows that CAD of solid pulmonary nodules using CT with chest x-ray equivalent radiation dose has similar sensitivities to CAD of solid pulmonary nodules with standard dose CT.
"Lowering radiation dose is a topic that is important for every radiologist as the numbers of CT performed each year have massively increased over the past decade. Thus, every attempt to lower the dose while maintaining an appropriate diagnostic quality is important," noted lead author Dr. Michael Messerli in an email to AuntMinnieEurope.com.
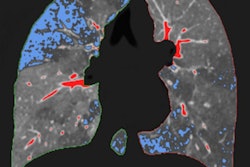
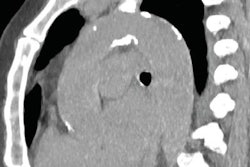
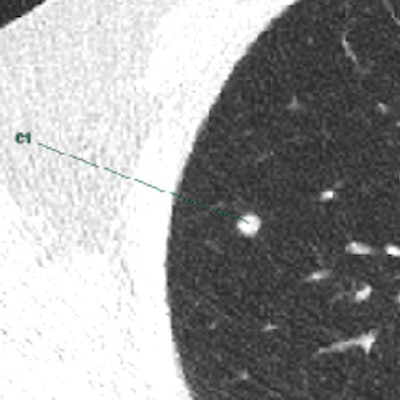
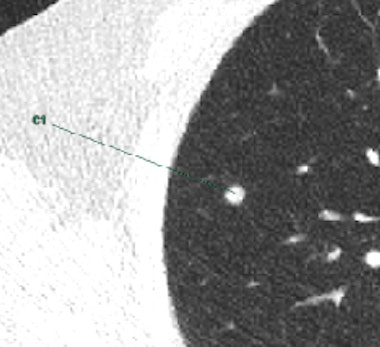 Marking of a CAD-software-detected solid nodule in the right upper lobe in ultralow-radiation-dose CT (0.15 mSv). All images courtesy of Dr. Michael Messerli.
Marking of a CAD-software-detected solid nodule in the right upper lobe in ultralow-radiation-dose CT (0.15 mSv). All images courtesy of Dr. Michael Messerli.Messerli, who won the best oral presentation Cum Laude award for the work at the 2016 annual meeting European Society of Thoracic Imaging (ESTI) in Krakow, Poland, sees two specific diseases where CAD in combination with ultralow-dose CT can improve patient handling.
"The technique might be used in a lung cancer screening setting, achieving a massive radiation dose reduction for the whole screened population. In addition, it might be of use for young oncologic patients -- for example, in seminoma cases -- who can profit from an early detection of potentially meaningful pulmonary nodules," said Messerli, a resident in the nuclear medicine department at University Hospital of Zurich. "I hope that CAD can be included smoothly in clinical workflows so that a time-efficient use can be ensured."
Clear results
The study involved 202 patients undergoing clinically indicated standard dose chest CT (1.8 ± 0.7 mSv) who were prospectively included and scanned with an additional ultralow-dose CT (0.13 ± 0.01 mSv) in the same session. The key results of the study are the following:
- The per-nodule sensitivity of CAD was 70% in standard dose CT and 68% in ultralow-dose CT.
- There was no significant difference in per-nodule sensitivity of CAD in standard dose compared with ultralow-dose CT both overall and in different size subgroups (all p > 0.05).
- Adding CAD markings in ultralow-dose CT significantly improved the sensitivity of two radiologists for detecting solid pulmonary nodules from 77% to 88% and from 66% to 79%, respectively.
- CAD can serve as an excellent second reader for nodule detection in CT even at dose levels similar to chest x-ray.
Consensus reading of standard-dose CT scans was performed by two radiologists. CAD was then performed in standard-dose and ultralow-dose CT with two different reconstruction kernels. CAD detection rate of nodules was evaluated including subgroups of different nodule sizes (< 5, 5-7, > 7 mm). Sensitivity was further analyzed in multivariable mixed effects logistic regression.
The researchers found 279 solid nodules in standard-dose CT. Solid pulmonary nodules were found in 126 patients, whereas 76 patients were identified as having no solid nodules. There was no significant difference in overall per-nodule sensitivity of CAD with 70% in standard dose compared with 68% in ultralow-dose CT, according to the authors. CAD use also yielded similar sensitivities with standard and ultralow dose in different size subgroups (all p > 0.05).
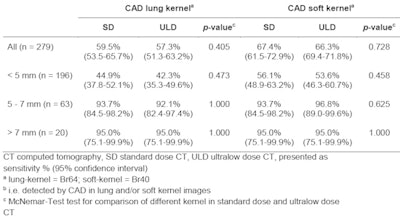 Per-nodule sensitivity for solid nodules of CAD in standard dose and ultralow-dose CT.
Per-nodule sensitivity for solid nodules of CAD in standard dose and ultralow-dose CT.CAD further led to a significant increase of sensitivity for both radiologists reading the ultralow-dose CT scans (all p < 0.001). After adding CAD results to their visual readout, sensitivity for detection of solid nodules was higher by 11.5% for reader 1 and 12.5% for reader 2, according to the paper. In multivariable analysis, the use of CAD (p < 0.001), and nodule size (p < 0.0001) were independent predictors for nodule detection; sensitivity increased with increasing nodule size. However, sensitivity was not influenced by BMI (p = 0.933) and the use of contrast agents (p = 0.176).
The authors described how 60% of the estimated 224,390 new cases of patients with lung cancer that are predicted to occur in 2016 in the U.S. are expected to be in an advanced stage. They state the National Lung Screening Trial (NLST) has suggested a reduced mortality from lung cancer among people at high risk that underwent low-dose CT. The authors believe it is likely CT will gain access to official screening programs for certain risk groups in the near future, subject to further studies on cost-benefits, and this means radiologists will play a vital role in early cancer detection and patient management.
Future applications
 Dr. Michael Messerli.
Dr. Michael Messerli.Messerli's ESTI 2016 lecture was called "CAD of solid pulmonary nodules in chest x-ray equivalent ultralow dose chest CT -- first in-vivo results at dose levels of 0.13 mSv." He is convinced while the technical part of the study might primarily be of interest to radiologists, such as what types of reconstruction kernel are best to use, the topic of the paper should also appeal to the wider healthcare community.
"As lung cancer screening is still a hot topic with ongoing debate, the drastically reduced radiation dose in combination with software-based nodule detection as performed in our study is definitely of interest for many healthcare professionals," he said.
He believes further studies should focus on the detection of subsolid nodules -- a morphologically different type than solid nodules -- because they seem to be more difficult to detect by CAD-software and probably also in ultralow-dose CT.
"There is definitely a case for inclusion in routine practice: The ultralow-dose CT might be used for detection and follow-up of lung nodules with different etiologies," he concluded.