
About 29% of practitioners don't disinfect ultrasound probes after each patient, 11% of practitioners fail to use a probe cover for transvaginal or transrectal procedures, and 30% don't use sterile gel sachets for endocavity scans, a new survey from the European Society of Radiology (ESR) has found.
The online survey was sent to 22,000 full ESR members in September 2015, and the response rate of completed surveys was 4.3% (946 practitioners, 97% of whom were radiologists, mostly working in larger hospitals). The survey results highlighted a wide range of ultrasound probe decontamination practices in Europe and showed that education is an urgent priority.
"These survey results underscore the importance of raising awareness amongst clinicians of the risks of infection associated with ultrasound, in particular when transducers are in contact with mucous membranes and potentially infected bodily fluids," noted lead author Dr. Christiane Nyhsen, consultant radiologist at City Hospitals Sunderland, U.K., and fellow members of the ESR Working Group on Ultrasound. "Expert European recommendations are needed to educate clinicians, guide best practices, and ensure that safe patient care is provided."
 Dr. Christiane Nyhsen.
Dr. Christiane Nyhsen.Although ultrasound is considered one of the safest imaging modalities, concerns have been raised about potential infection transmission risks, Nyhsen and colleagues wrote in an article published online on 24 October by Insights into Imaging. They designed a survey to establish infection prevention and control measures in ultrasound and also to highlight the importance of good medical practice.
Using the SurveyMonkey software, a total of 22 questions were posed about the country and city of work, the work setting (private center versus hospital), size of the establishment, and number of yearly ultrasound procedures undertaken. Known incidents involving transmission of infection were queried with free text available for further clarification. The final part of the survey gathered data on the gel used both in direct contact with the patient and inside probe covers.
The largest number of respondents came from Italy, U.K., Spain, and France. The majority of survey respondents worked exclusively in a hospital (81%); the remainder worked in private centers or offices (15%), and 4% indicated mixed/other work commitments. Most practitioners (67%) worked in relatively large institutions (100 to 1,000 beds), with 16% working in very large hospitals with more than 1,000 beds. Also, 12% had no patient admission facilities. The majority (88%) performed over 3,000 ultrasound exams per year, with 42% of the institutions carrying out more than 10,000 annual scans.
Almost all surveys were completed by radiologists (97%). Eight responses in total were received from cardiologists, gynecologists/obstetricians, and urologists. Twenty respondents stated mixed practice or work in other specialties such as breast services, pediatrics, or emergency medicine.
Summary of key findings
Some of the main results were as follows:
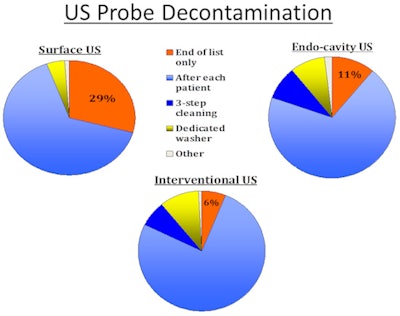
- Almost two-thirds of respondents decontaminated the probe by wiping off the gel first, with subsequent disinfection of probes with foam or wipe after each patient (618, 65%), while 276 (29%) disinfected the probes only at the end of the list of patients. Only 4% used a dedicated washer to thoroughly decontaminate probes in this setting. Some practitioners wiped the probe with a dry towel, but they took no subsequent disinfection measures.
- When the patient was known to have a transmissible infection, 724 (77%) wiped off the ultrasound gel and then used disinfecting wipes/foam after the procedure, and 174 (18%) cleaned the probe in a dedicated washer. Also, 48 (5%) detailed other procedures or gave insufficient information.
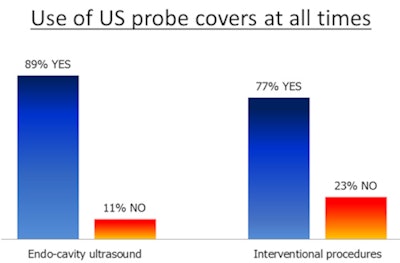
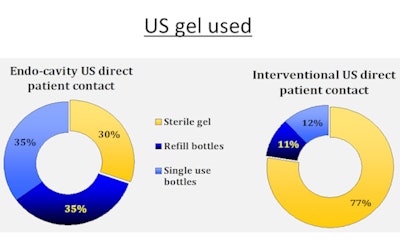
- About 70% of the sample performed interventional procedures. Of these 666 interventional practitioners, the majority used probe covers at all times (513, 77%), while almost one-quarter (153, 23%) did not. The gel inside the probe cover used for interventional procedures was typically from either a refill bottle (269, 40.4%) or a single-use bottle (229, 24.4%), while 168 (25.2%) used sterile sachets. Ultrasound gel used in direct contact during interventional procedures was mostly from sterile sachets (516, 77.5%). The remainder stated they used gel from refill bottles (70, 10.5%) or single-use bottles (80, 12%).
- Probe decontamination procedures were similar to endocavity probe disinfection, with most practitioners wiping off the gel with subsequent disinfection after each patient (507, 76%), while 47 (7%) used a thorough three-step high-level disinfectant wipe cleaning process, and 66 (10%) used a dedicated probe washer.
- Twenty-six practitioners knew of cases of infection transmission through ultrasound procedures, proving this is a topic worth considering. The actual figure of ultrasound probe contamination and transmission of infection is unknown and is potentially higher, as an estimated risk study from France shows, even though another French study did not find an increased risk of acquired HIV or hepatitis C infections following transvaginal procedures.
- The choice of ultrasound gel is another factor. Gels used for medical purposes do not have bacteriostatic properties per se, and they cannot be viewed as sterile unless specifically stated by the manufacturer. In the survey, a minority of practitioners used sterile gel sachets in direct patient contact for endocavity scans (30%), while the majority used sterile gel for interventional procedures (77.5%).
Complete decontamination of ultrasound transducers is challenging, conceded Nyhsen and her colleagues. Wiping probes with a dry towel can result in persistent contamination, and many potent and proven in vitro effective chemical disinfectants, such as glutaraldehyde, can pose health hazards to staff in direct skin contact or through inhalation, as well as causing unhealthy work environments for staff and patients.
In addition, the nature of the probe surface and its susceptibility to damage by chemicals -- for example, alcohol -- must be considered. Manufacturers should provide detailed information on which disinfectants are compatible, and they should be prepared to provide further product testing upon request.
The authors acknowledge that implementing any additional infection prevention measures will not be cost-neutral. Capital investment for additional transducers and decontamination equipment may be needed, and there will be higher ongoing costs for probe covers and sterile gel. All staff working in ultrasound departments must be adequately trained in using the available resources as effectively as possible, they pointed out.
The involvement of a very experienced professor of microbiology (Dr. Hilary Humphreys from the Royal College of Surgeons in Ireland, RCSI Education & Research Centre, Beaumont Hospital in Dublin) was invaluable in analyzing this survey, Nyhsen told AuntMinnieEurope.com. Raising awareness is important, and much more needs to be done. The other co-authors were Dr. Michel Claudon from Nancy, France, chairman of the ESR Working Group on Ultrasound; Dr. Carlos Nicolau from Barcelona, Spain; and Dr. Gerhard Mostbeck from Vienna.
Looking ahead, the authors now are working on establishing best practice recommendations to guide all ultrasound practitioners in various settings. These will be presented at ECR 2017, where a lunchtime session is scheduled and will also include presentations from patient and industry representatives, with constructive discussions at the end.



















