Some endovaginal ultrasound probes are not correctly disinfected, and the medical imaging community must develop an easy and fast disinfection protocol without compromising quality, according to an article published in the Israel Medical Association Journal.
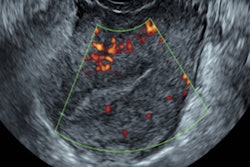
Endovaginal ultrasound is widely used in obstetric and gynecological imaging, allowing for the evaluation of disease in the female reproductive tract and fetal surveillance during all stages of pregnancy. But concern has been rising about the possibility of transmitting infection via internal probes such as endovaginal transducers, wrote a team led by Dr. Chen Ben David from Rambam Health Care Campus and Technion - Israel Institute of Technology in Haifa.
"The main concern is that these probes may enable contamination by pathogenic microorganisms and, therefore, act as vectors, transmitting pathogens among patients," the group wrote (Isr Med Assoc J, January 2019, Vol. 21:1, pp. 45-49).
Contamination under scrutiny
The problem isn't unique to Israel: Internal probe contamination has been under scrutiny around the world. Last fall, a Pennsylvania hospital in the U.S. faced legal action because improperly cleaned ultrasound probes were used on more than 200 patients for prostate or ob/gyn exams. And a 2016 survey conducted by the European Society of Radiology (ESR) found that almost a third of practitioners don't disinfect transducers after each patient, and 11% don't use probe covers for transvaginal or transrectal procedures.
The vagina hosts many microorganisms, most of which serve as a defense against genital infections. But some have the potential to cause vaginitis, urinary tract infections, or pneumonia and to infect women with hepatitis, HIV, and HPV. That's why proper cleaning of the probes is crucial, the researchers wrote
A common safety measure for endovaginal probes is the use of probe covers. But these still carry a slight chance of rupture during procedures, which has prompted the U.S. Centers for Disease Control and Prevention (CDC) to recommend using high-level disinfectants in addition to probe covers after each patient. (American, Canadian, Australian, and Scottish medical societies have published similar guidance, the researchers noted.) High-level disinfectants destroy most microorganisms, except for those that form endospores.
In 2017, the Israeli Ministry of Health released guidelines for the proper handling of endovaginal ultrasound probes that followed the CDC's recommendation. The guidelines included the following instructions:
- Remove the probe cover.
- Change gloves after cleaning hands.
- Clean the probe with special wipes.
- Clean the probe with a high-level disinfectant using either a chemical or physical method (ultraviolet light).
But many ob/gyn ultrasound departments find it difficult to adhere to these requirements because the process takes time: The disinfectant must dry or dissipate before the probe can be used on the next patient, corresponding author Dr. Ido Solt told AuntMinnie.com via email.
"As physicians who work in busy gynecological ultrasound units, we have noticed that physicians find it very difficult to adhere to this strict disinfection protocol between each patient," he said.
What's the actual risk?
Studies conducted to establish the risk of contamination of endovaginal probes -- despite the use of probe covers -- have found a range of 0.98% to 3.4% for bacterial contamination and a range of 1.5% to 14.2% for viral contamination, the researchers wrote. But since there is little research on the actual risk of infections among women exposed to contaminated vaginal probes, probe cleaning guidelines are based on the theoretical risk of contamination.
 Dr. Ido Solt from Rambam Health Care Campus.
Dr. Ido Solt from Rambam Health Care Campus."Despite reported risks for contamination of endovaginal ultrasound probes and their frequent use in daily practice, there are few published reports regarding infections arising subsequent to those examinations," the researchers wrote.
The Israeli Ministry of Health's guidance on the issue relies on the CDC standards and is based on the risk of probe failure -- which, actually, rarely occurs, according to the group. That leaves practitioners in a quandary.
"Currently, it is almost impossible to pragmatically adhere to the Israel Ministry of Health guidelines," the researchers wrote.
What's needed is further research on the actual incidence of infections transmitted through vaginal probes, which can then inform best-practice protocols for the disinfection of vaginal ultrasound transducers, Solt told AuntMinnie.com.
"We need to develop an easy and fast disinfection protocol without compromising disinfection quality," he said.