Undercapacity in radiology departments is leading to substantial costs for hospitals because imaging delays significantly prolong in-patient length of stay, but the problem can be solved by hiring more staff to run existing equipment for longer, according to researchers from a leading Irish facility.
"Our hospital [imaging service] is underprovided, and we wanted to show what the downstream cost of this is to the hospital," said Dr. Niall Sheehy, head of radiology at St James' Hospital (SJH) in Dublin. "At the moment from a financial standpoint, radiology is considered a cost, so we need to show that it is a benefit, and that it is more cost-effective to perform quicker tests, rather than keeping patients in expensive beds waiting for tests."
 Dr. Niall Sheehy, St. James' Hospital, Dublin. Image courtesy of Royal College of Surgeons in Ireland, Faculty of Radiologists.
Dr. Niall Sheehy, St. James' Hospital, Dublin. Image courtesy of Royal College of Surgeons in Ireland, Faculty of Radiologists.The longer inpatients remain in hospital waiting for a scan, the higher the cost of bed stay, currently estimated at around 1,000 euros per night in Irish hospitals. Imaging tests are significantly cheaper than this, for example a standard MR exam costs as little as 200 euros, Sheehy and his colleagues noted.
While MRI, ultrasound, and CT demand at SJH has increased by 19%, 11%, and 22% respectively between 2010-2014, the average number of radiologists in Ireland and the U.K. are just over half of the European average. The number of radiographers is similarly reduced. This staffing deficit, rather than an equipment shortage, is the limiting factor for imaging capacity. Certain modalities, like MRI, have only sufficient staff to run a five-day service.
The SJH team used a study model that factored in the degree of patient illness to show it was not just the sicker patients that stayed longer and underwent more imaging tests, but that time to the imaging test correlated to length of stay for all patients, compared with those who were not booked for imaging.
"We found that among patients who had the same degree of illness, those who had no imaging tests ordered went home sooner than those that underwent imaging tests," Sheehy explained. "It is important for health service planners, hospital fund managers, finance officers, and radiology department directors to understand that imaging is directly prolonging length of stay for patients because it has insufficient capacity. An underfunded radiology department is a big source of inefficiency and increases overall costs."
Although the research group knew that delayed imaging was prolonging patient hospital stay, the degree to which it impacted bed days came as a surprise. Even relatively low morbidities experienced longer admissions. For example, patients booked for a brain MRI to diagnose cause of seizure would be bumped in the queue for someone "sicker" and consequently their stay in hospital could be prolonged by several days, he added.
The next step locally is to use the same model to show how prompter scanning would impact costs. Decreasing turnaround time to 24 hours for MR, for example, should mean that imaged patients stayed in hospital for a similar amount of time as nonimaged patients, and the authors will be able to determine how many bed days, and their cost in Euros, this will save.
"By showing in concrete terms, the potential gain in bed days, and financial savings, we are trying to locally make a case for more investment in imaging," Sheehy noted.
Study logistics
Early imaging has been associated with shorter hospital stays, improved patient outcomes, and lower overall costs, but to date, the literature, has been lacking in quantitative analysis, relating to turnaround times and length of stay. The group's latest study, published online by Clinical Radiology on 19 May, may be among the first quantitative studies proving that neglected and underfunded imaging services hamper efficiency.
The study evaluated all emergency admissions to St James' hospital totaling 25,326 imaging investigations (20,504 patients) during the years 2010-2014 and examined the extent to which time to completion for CT, MRI, and ultrasound could be shown to influence the hospital length of stay while accounting for patient acuity. The authors adjusted estimates of risk (odds or incidence rate ratios [IRRs]) of the regressors for acute illness severity, charlson comorbidity, chronic disabling disease score, and sepsis status.
Increased imaging reflected clinical complexity -- mortality increased with the number of investigations from none (3.5% mortality), CT alone (5.4%), or both ultrasound and CT undertaken (9.5%), according to the study. In the whole patient group, length of stay showed a similar finding, with an increase in length of stay from 4.0 days for those with no investigations to 18.4 days for patients undergoing both ultrasound and CT exams. According to the authors, the most significant finding was that after adjustment for clinical complexity, the time to completion of imaging for each of CT, MRI, and ultrasound remained an independent predictor (p < 0.001) of length of stay.
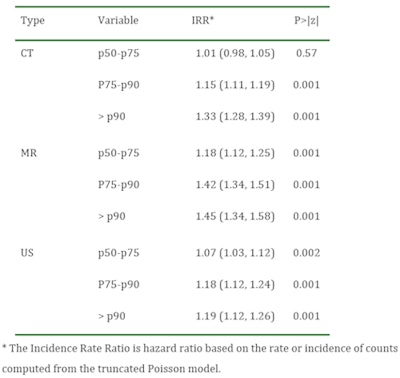 Multivariable adjusted Poisson model for total hospital. Length of stay cutoffs refer to the 50, 75, and 90th centile of the time distribution from order to completion for each imaging modality.
Multivariable adjusted Poisson model for total hospital. Length of stay cutoffs refer to the 50, 75, and 90th centile of the time distribution from order to completion for each imaging modality."After you have looked at the most efficient use of your existing staff and educated the referring clinicians in the best use of radiological investigations, the only way to tackle the delays and to curb costs is to hire more staff to run modalities for more hours," Sheehy commented. "There should be routine access to both CT and MR for seven days a week, not five days with emergency access only at night and over the weekend as is currently the case. Prompter scanning would obviate keeping patients in beds who are not ill and who should go home."
The authors said the paper is hopefully the beginning of a wider study that will analyze admissions and discharge data from the national PACS, which serves multiple hospitals across the Republic of Ireland. Because the group had access to St. James' laboratory data, the authors were able to categorize patients by clinical complexity. This categorization might be more difficult in the larger multisite study but could be achieved to an extent through analysis of discharge coding. It is hoped a national laboratory information system, now in its infancy, will enable this type of large-scale data extraction in the coming years.
Activity-based funding
Sheehy described how Irish hospitals are changing their funding model from an annual block grant to reimbursement by diagnosis-related group, this model known as "activity-based funding." Internationally, other health systems that used to fund radiology on a fee-per-item basis are switching to diagnosis-related group-based reimbursement. Under this system, reimbursement to the hospital is based on a patient's diagnosis and morbidity, not on how many days they were in hospital or how many tests or procedures were performed.
"On the basis of this reimbursement model, hospital financial directors may attempt to withdraw funding from radiology, as imaging tests can be seen as costs that do not contribute to income. This study shows that this strategy may end up costing the hospital far more overall -- with significant costs associated with length-of-stay -- than any savings made in radiology," he concluded.



















