Investigators are envisioning a brave new world in which functional 3D-printed organs can be manufactured at low cost for implantation in patients -- provided several tough obstacles can be overcome, concludes new research from a top London institution.
The development of functional organs from 3D printed materials is showing promise despite daunting challenges, most importantly in the development of advanced printing materials that can be used in organ scaffolding, and vascularization of the new organs.
"Three-dimensional printing is a fascinating new technology that could revolutionize treatment of cardiac interventions," wrote co-author Alexander Seifalian, PhD, professor of nanotechnology and regenerative medicine from the University College London's (UCL), in an email to AuntMinnieEurope.com.
"The ultimate goal is to achieve the development of functional human organs and tissues, to overcome limitations of organ transplantation created by the lack of organ donors and life-long immunosuppression," wrote Dina Radenkovic and Seifalian from UCL and Atefeh Solouk, PhD, from Amirkabir University of Technology in Tehran (Medical Hypotheses, February 2016, Vol. 87, pp. 30-33).
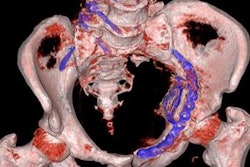
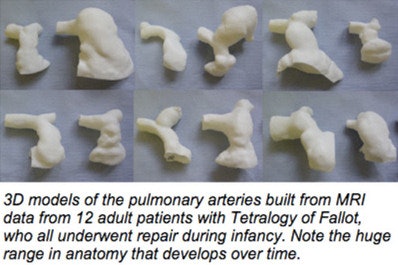
CT and MRI are at the heart of rapid prototyping of 3D models for 3D printing, which has become a fast-growing additive manufacturing industry, the authors wrote. The technology is already being used in myriad applications used in surgical planning or high-risk operations.
"The first clinical application has been to print models of patients' heart valves, blood vessels, or other organs for the clinician ... to help deliver endovascular devices," Seifalian said. "Here in the U.K. at Great Ormond Street Hospital for Children, it is common practice for delivery of transcatheter heart valves. The dataset required for 3D printing currently are from CT or MRI."
Much more complex organ printing is possible if a number of substantial barriers can be overcome.
"Actual 3D printing of cardiovascular devices such as heart valves, stents, or coronary bypass grafts is not here yet," Seifalian stated. "The materials used to manufacture heart valves or bypass grafts cannot be printed with the 3D printer. Although in early experiments, researchers are printing cells and scaffolding in heart valve tissue engineering or cardiac patch, I cannot foresee it clinically in the next 10 years."
At the same time, technology is advancing every day with new biomaterials being developed for use in printing organs. Solving the technical hurdles would transform what is still science fiction into the reality of 3D printing of functional human organs, the authors wrote.
Transplantation untenable
The need for rapid development of this technology is acute, with rising organ shortages and the growing needs of an aging population, the team wrote. A shortage of donors, high transportation costs, the need for immunosuppression, morbidity, and mortality are just a few of the problems. Doctors can also spend years searching for a suitable transplantation donor, only to find out that a donor and recipient aren't biocompatible.
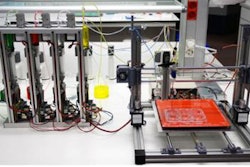
New printers
Several new printer technologies could help nudge organ printing forward, including cost-efficient ink-jet printers with small droplet size and low viscosity. Microextrusion printers are slow and expensive, but feature continuous release of materials. Tissue diversity can expand with greater use of biologic materials like collagen, hyaluronic acide, alginate, chitosan, and thermoplastic synthetic polymers like polyurethane and polylactic acid, they wrote.
Personalized 3D printing could transform plastic and reconstructive surgery. Moreover, the introduction of 3D-printed blood vessels instead of transplanted vascular grafts could change our approach to cardiovascular pathologies, suggest the authors, who advocate an initial focus on human hollow organs of lower architectural complexity such as arteries, trachea, larynx, urethra, bile ducts, and facial reconstruction of ears and noses, using detailed information from advanced imaging, 3D printing, and appropriate cell types. Such methods would enable a novel precision medicine approach in surgery.
Tissue engineering
Tissue engineering is a rapidly advancing field involving the use of a biocompatible tissue scaffold loaded with a several cell types including stem cells that are capable of self-renewal and regeneration, differentiated mature cells, or a mixture of differentiated cells, the authors noted.
Lately, researchers have poured money and effort into the development of synthetic or biological scaffolds, including a synthetic trachea using nanocomposite material created in the authors' laboratory, and a lacrimal duct created with collaborators at University Hospital Zurich, they wrote. But difficulties in scaffold manufacturing have prevented the establishment of robust clinical techniques.
Three-dimensional printing could change all that, by mimicking the characteristics and geometry of the target tissues, the authors wrote. Problems with manual cell seeding would be eliminated, and models would have easily reproducible and standardized pore sizes to facilitate cell proliferation and aggregation. By combining biological and synthetic bioresorbable materials, 3D-printed scaffolding could even have higher load-bearing properties than human tissue.
Preventing cell death during heating and printing of the scaffold is a challenge, but several researchers reported that cell viability can be restored by incubation in a medium after 3D printing.
Skin, liver, neuronal tissue, muscle-tendon units, and cartilage have already been created successfully. But big problems remain to be overcome, including the need to vascularize the graft. Grafts could potentially be placed in close proximity to the vessels and connected by vascular surgery, or better yet, designed with vessel networks already incorporated.
- A 3D printed aortic sleeve has been used in a clinical setting rather than as a vascular graft. Researchers from the University of Michigan successfully implanted a bioresorbable 3D-printed tracheal splint created using microextrusion bioprinting for use in a child with severe tracheomalacia, the authors wrote.
- Custom facial bones created with ink-jet printing are becoming a standard of care for maxillofacial surgery in Japan, and researchers in the Netherlands have performed total jaw and skull reconstructions using custom 3D implants by Xiloc Medical. Cybernetic experiments have been used to create 3D-printed bionic ears
"If medicine keeps up with the advances in a high-technology field, we could have synthetic 3D-printed ears that hear and a nose with a sharp sense of smell," they wrote. The group is currently collaborating with Indian researchers to develop tissue-engineered auricles using 3D printing for scaffold processing. In the near future, these products could be used to reduce the stigma and burden of multiple surgeries in patients with microtia.
Financial barriers
Beyond technology hurdles, the cost of functional organs may be too high for clinical use, Radenkovic and colleagues wrote. A tracheal split might cost $100 (90 euros), but a nose more like $40,000 (36,000 euros). Bioprinting of live cells using biological materials could reach $300,000 (272,000 euros).
This multidisciplinary field will require scientists, engineers, software developers, and physicians to join forces and work on it together, they wrote. Technological advances will certainly reduce the cost of 3D printing.
More research is needed on the interaction between humans and printing materials with the goal of standardizing materials and allowing the optimal time for the maturation of fabricated tissues.
"Lastly, scientists and engineers must restore some organ functionality and solve the problem of vascularization to enable 3D printing of more complex organs," the team wrote.