
Time and money spent monitoring every patient with a hip prosthesis could be saved by using a routine radiostereometry imaging procedure to assess prosthesis migration, according to a Swedish expert.
The technique is around 40 years old, but its use for assessing patients who have been through a second hip operation remains at research level, despite highly successful outcome prediction rates, said Dr. Maziar Mohaddes, PhD, consultant orthopedic surgeon at Sahlgrenska Academy, University of Gothenburg. Furthermore, the methodology can also be applied to knee implants and spinal, pediatric, and trauma orthopedic surgery.
 High resolution x-ray shows prosthetic hip implant. The white dots are the tantalum markers that will create polygons between bone and implant. All images courtesy of Dr. Maziar Mohaddes, PhD.
High resolution x-ray shows prosthetic hip implant. The white dots are the tantalum markers that will create polygons between bone and implant. All images courtesy of Dr. Maziar Mohaddes, PhD.In Sweden alone, around 16,000 hip prosthesis operations are performed annually. There are also an estimated 1,100 reoperations to replace or remove part or all of the three-part implant that comprises a plastic socket, a metal femoral head, and a metal stem inserted into the thighbone. Between 5% and 30% of those who receive a new hip prosthesis will require a reoperation during their lifetime. The risk of reoperation varies with the patient's age: around 30% of patients younger than 50 must undergo a reoperation within 15 years, while the corresponding figure for those older than 75 is 5% to 10%.
It is these reoperated patients that have been the focus of research by Mohaddes, who recently successfully defended his PhD thesis on this topic. In his research, he insists that the high-resolution x-ray method, radiostereometry, is 10 times more accurate than plain x-ray for detecting implant motion, and migration measured with radiostereometry can predict which patients have the greatest risk of further reoperation.
The technique can only be deployed if during hip surgery tantalum markers are placed in the implant. Ten markers are inserted in the femoral bone, 10 in the plastic hip socket, and 10 in the pelvic bone. Soon after surgery, the patient is x-rayed, this against a reference plate and with two beams so that he or she can be correlated with the room. The markers create polygons inside the bone and in the implant. These polygons are imaged periodically so that any movement between the bone markers and prosthesis markers can be visualized. This movement can then be compared postoperatively from one exam to another over a period of time.
"The methodology can also be applied to knee implants, spinal, pediatric, and trauma orthopedic surgery," Mohaddes added.
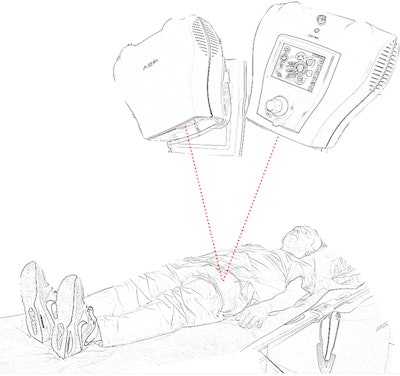 Illustration of the technique for monitoring prosthetic migration: Soon after surgery the patient is x-rayed against a reference plate with two beams. The tantalum markers in the bone and implant create polygons which show any movement over time when imaged periodically.
Illustration of the technique for monitoring prosthetic migration: Soon after surgery the patient is x-rayed against a reference plate with two beams. The tantalum markers in the bone and implant create polygons which show any movement over time when imaged periodically."At the next follow-up exam, three months postoperative, the patient may be asymptomatic, but we can at this stage assess whether the patient will need yet another surgical intervention in the future. However, my research has shown that it is radiostereometry examination at two years that is the most accurate predictor of outcome. Previous research in primary cases has shown that if the prosthesis has moved by more than 1 mm at two years, risk of reoperation is increased by 15%" he told AuntMinnieEurope.com. "The two-year value of migration is even more prognostic in revision cases. If the patient has already been reoperated and the prosthesis moves 1 mm in the first two years after the latest surgery, the risk of reoperation increases twofold."
The sensitivity of radiostereometry is high, and movement of 0.2 mm can be detected using such analysis, compared with movement of about 2 mm by conventional x-ray alone.
The Swedish scene
In Sweden, primary hip operation patients are not monitored by x-ray but by patient-reported outcome measure forms. Conversely, most revision patients are followed regularly by x-ray during their lifetime. Although the intervals grow further apart, many patients are being needlessly monitored.
"By using radiostereometry we can find the patients needing close monitoring and in whom any symptoms should be dealt with immediately, then the majority of operated patients can be kept out of the office, better for the healthy patient and for the health system," Mohaddes said.
 Clinical application of the new x-ray technique may avoid needless monitoring of revision patients who show no sign of prosthesis migration after two years postoperative, according to Dr. Maziar Mohaddes, PhD.
Clinical application of the new x-ray technique may avoid needless monitoring of revision patients who show no sign of prosthesis migration after two years postoperative, according to Dr. Maziar Mohaddes, PhD.The reliability of prediction has pushed the team at Sahlgrenska to question whether clinical routine should be changed for asymptomatic revision patients in whom there is no prosthesis migration, so that instead of coming back for radiological exams over their lifetime, these checks can end at two years unless symptoms develop.
Furthermore, in the revision patient who presents with prosthetic movement while asymptomatic, early detection should result in easier reoperation and probably easier rehabilitation before any serious destruction of the bone occurs, he pointed out.
Among its other benefits is that radiostereometry uses significantly less radiation than plain x-ray as it is more sensitive and therefore quicker at detecting the tantalum markers.
The research team at the joint replacement unit in Sahlgrenska is considering applying for ethical approval for all revision patients to be implanted with markers during surgery so that such monitoring can become clinical routine. Mohaddes points to a hospital in Denmark that has been granted permission to use the technique in routine practice for hip fracture patients operated with a hip prosthesis. Ethical approval would apply to all hospitals in the region, although only those that could house the specific laboratory required, namely the larger hospitals that perform orthopedic surgery, would be able to use the technique on their patients.
In addition, there needs to be an economic study to find out how much the health system would stand to gain from deploying the technique in regional hospitals in order to gain administrative approval, he concluded.



















