FDG-PET strongly predicts overall survival in patients suspected of having early-stage atypical Parkinsonian syndrome (APS), according to a study in the October Journal of Nuclear Medicine. The modality's findings closely matched clinical diagnosis at one-year follow-up.
In a comparison of patients with atypical Parkinsonian syndrome or similar forms of dementia, PET predicted a significantly shorter survival time of 4.1 years from the time of the initial PET scan for those with APS. Most interestingly, PET's prognostication matched survival time as determined by the clinical diagnosis at one year of follow-up.
The research "strongly supports" using PET early in a patient's workup to make decisions about his or her treatment strategy, clinical trial participation, and counseling, concluded the group led by Dr. Sabine Hellwig from the University Hospital of Freiburg in Germany.
"Overall, these are remarkable results if one considers that the clinical diagnosis was finalized after a median follow-up of one year after the PET scan," the authors wrote (JNM, October 2015, Vol. 56:10, pp. 1541-1546).
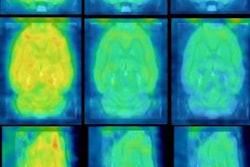
Detection with PET
Early detection of atypical Parkinsonian syndrome and differentiating the condition from similar dementia is critical because APS can rapidly lead to disability and death, the group wrote.
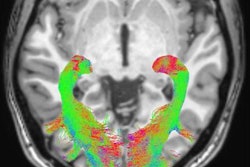
FDG-PET's ability to discern between different disease patterns of regional cerebral glucose metabolism makes the modality particularly helpful in differentiating atypical Parkinsonian syndrome from other afflictions.
In fact, PET has been known to confirm as many as 80% of clinical diagnoses of Parkinson's disease, atypical Parkinsonian syndrome, and other neurological conditions, such as Lewy body disease, multiple system atrophy, progressive supranuclear palsy, and corticobasal degeneration. Given those results, many researchers assume that PET also carries prognostic capabilities.
"However, this rationale is challenged by the limited accuracy of the clinical diagnosis compared with the diagnosis at autopsy (70%-75%), which implies that the correctness of the diagnosis or prognosis given by PET is ill-defined," the authors wrote.
Therefore, Hellwig and colleagues sought to answer the question of how well FDG-PET can predict survival for patients with clinically suspected atypical Parkinsonian syndrome.
The study cohort consisted of 78 patients referred for diagnostic imaging between July 2008 and January 2011 for clinically suspected but unconfirmed early-stage APS. The subjects were followed for up to 5.9 years after PET imaging.
Among the 78 subjects, 44 were diagnosed with atypical Parkinsonian syndrome and 34 had Lewy body disease, the second most common form of progressive dementia after Alzheimer's. Two board-certified neurologists made their clinical diagnoses of either APS or Lewy body disease after a median follow-up of 12 months (the minimum was six months).
Two investigators blinded to the clinical data independently interpreted the PET scans, which included standardized transaxial and sagittal images and 3D stereotactic surface projections to show each subject's cerebral FDG uptake. PET imaging was performed at the start of the study and at the one-year follow-up.
Survival rates
Of the original 78 subjects, 44 were still alive at the median follow-up duration of 4.7 ± 0.6 years after initial imaging.
Patients diagnosed with atypical Parkinsonian syndrome by PET or at their one-year clinical follow-up showed a significantly shorter median survival time, at 4.1 years, than patients with Lewy body disease, who had not yet reached median survival.
Further analysis of survival time showed that one year after the initial PET scan, 27 (61%) of the original 44 patients with APS had died, compared with seven (21%) of the 34 Lewy body disease patients.
At two years, 15 (89%) of the 17 surviving APS patients were still alive, compared with 25 (94%) of the 27 survivors with Lewy body disease. After four years, only nine APS patients were still alive, compared with 23 of those with Lewy body disease.
As mentioned earlier, Hellwig and colleagues described the results as "remarkable," given that the clinical diagnosis was finalized after a median follow-up of one year.
"A time span of one year (or 25% of remaining life expectancy) typically corresponds to a relevant disease progression in APS, which would be expected to translate into a higher diagnostic and prognostic clinical confidence," they added.
The authors believe that the study is the first to compare the prognostic value of PET and clinical diagnosis.
In addition, by focusing on PET's ability to predict survival and selecting a hard clinical end point, they demonstrated that "PET is a prognostic marker on its own," circumventing previous concerns about the accuracy of clinical diagnosis and its use as a reference standard, according to the group.
"Risk stratification by FDG-PET appears to be at least as predictive as the one-year follow-up clinical diagnosis," they concluded. "This finding strongly supports the early inclusion of PET imaging in patient care to aid decisions on treatment strategies, clinical trial participation, and prognostic counseling."