The European CARDIS project aims to use silicon photonics to allow large-scale screening of populations for cardiovascular disease (CVD) risk.
According to the World Health Organization (WHO), cardiovascular disease is the No. 1 killer in the world today. In 2012, around 17.5 million people died from CVDs, such as heart disease and stroke, accounting for more than 30% of all global deaths. CVDs can be diagnosed using various tools, including chest x-ray, electrocardiogram, Holter monitoring, and cardiac MRI. However, for early predictions of CVD risk in large populations, these tools are either too complicated or too expensive. As a result, individuals with a risk considered to be low or moderate are often undiagnosed.
A consortium of companies and research institutes, led by IMEC in Belgium, has recently been awarded 3.6 million euros from the European Commission's Horizon 2020 program to develop a mobile, low-cost, noninvasive, point-of-care screening device. Called CARDIS, the project kicked off in February and will run for 42 months with the aim of making CVD mass screening possible.
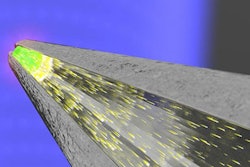
It is based on technology called laser Doppler vibrometry (LDV) -- a noncontact technique that directs a laser at a moving surface and then uses the Doppler shift of the reflected light to infer its vibration amplitude and frequency. This technique has already been used in applications such as aircraft inspection and the monitoring of hard-disk drives, but only recently has it been used for CVD studies.
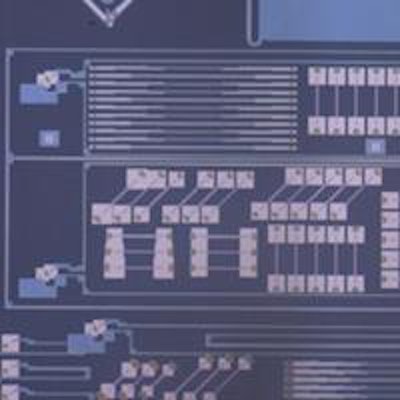
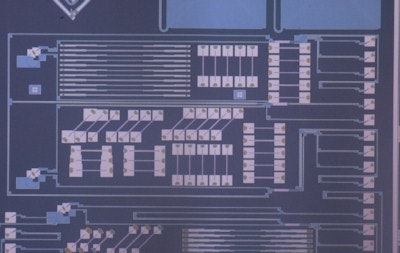 One of the silicon photonics chips used for the laser Doppler vibrometry project. Image courtesy of Roel Baets.
One of the silicon photonics chips used for the laser Doppler vibrometry project. Image courtesy of Roel Baets.As part of the CARDIS project, LDV is used to detect vibrations of certain locations on the skin close to arteries or on the chest. The idea is to retrieve a number of useful parameters used for CVD screening, one of the most important being arterial stiffness. A stiffer artery leads to a higher pulse wave velocity -- the velocity of the pressure pulse in the arteries caused by the beating of the heart -- so by measuring the pulse wave velocity, arterial stiffness can be assessed.
This measurement is typically made by recording how long it takes a pulse wave to travel between two different locations along the same artery. Although various vibration sensors can be used for this measurement, LDV can operate without physical contact and with higher accuracy.
Laboratory success
Studies have shown that LDV is sensitive enough to pick up additional information linked to CVD risk, such as stenosis-induced vibrations and cardiac-contraction abnormalities. Because commercial LDV devices contain discrete optical components or fiber systems that make them bulky and expensive, such LDV-based assessment has so far been limited to laboratory conditions. But this type of assessment has already been included in the 2013 guidelines for CVD risk prediction drawn up by the European Society of Hypertension and the European Society of Cardiology.
The feasibility of the LDV technique was demonstrated in a small-scale study several years ago by the present authors and colleagues (American Journal of Hypertension, October 2011, Vol. 301:4, pp. H1389-H1395). Following this, Yanlu Li -- a graduate student from Ghent University in Belgium -- worked for four years to develop an on-chip version of LDV (Optics Express, Vol. 21:11, pp. 13342-13350).
CARDIS is the natural successor to this work and will bring the technology to a European level. The key innovation behind it is the use of silicon-based photonic integrated circuits, which can be manufactured in high volume and at low cost in the same fabrication plants that make computer chips. Indeed, the small (< 1 mm2) footprint of a single on-chip device means it is just as easy to make a chip holding, say, 10 LDV circuits as it is to make a single circuit.
In 2013, we demonstrated in vivo pulse wave velocity measurement with an on-chip double-LDV system (Biomedical Optics Express, Vol. 4:7, pp. 1229-1235), where the "double" refers to its need to measure skin movement at two locations. With CARDIS, in contrast, the proposed pulse wave velocity measurement device will be a photonic chip with two groups of six LDV systems. A custom-designed micro-optic system will focus the six beams on the skin to ensure that at least one spot is located on top of the artery, offering a user-friendly device that allows a doctor or a nurse to assess CVD risk in less than a minute.
Silicon photonic integrated circuits have a lot of potential for other demanding sensor applications for clinical diagnosis, such as sensing glucose levels in the interstitial fluid of diabetes patients. In this application, which our group has shown could work, the chip would be the heart of a compact subcutaneous implant.
The CARDIS project is well-placed to succeed, boasting institutes with a track record in cardiovascular research and clinical validation, including Ghent University, Maastricht University in the Netherlands, INSERM in France, and Queen Mary University of London in the U.K. On the technology side, IMEC, SIOS Messtechnik in Germany, and the Tyndall National Institute at University College Cork in the Republic of Ireland, will work to design the system and the photonic chip, and to integrate all the components in a compact device. Meanwhile, Netherlands-based Medtronic brings expertise in developing medical devices and bringing them to market.
The outcome of CARDIS will be a complete, functional prototype. Turning this into a commercial device that can be manufactured in high volume is beyond the remit of the project, but our results should encourage industry to invest on its own.
Roel Baets, PhD; Patrick Segers, PhD; and Danae Delbeke, PhD, are from Ghent University in Belgium. Baets is a professor in the department of information technology and a member of the Plateau Photonics Innnovation Center Photonics Research Group. Segers is a professor in the department of electronics and information systems and a member of the Institute Biomedical Technology (IBiTech) bioMMeda research group on biofluid, tissue, and solid mechanics for medical applications. Delbeke is a photonics technology developer with the Plateau Photonics Innnovation Center.
This article originally appeared in Physics World: Focus on Optics & Photonics.
© IOP Publishing Limited. Republished with permission from Physics World.