In a new audit of musculoskeletal (MSK) errors made at a top London hospital, the most common mistakes presented at discrepancy meetings in 2014 were wrist fractures, with triquetral fractures being the biggest group within these, and the most common type was perceptual.
Researchers from King's College Hospital found that the data for the preceding year (2013) showed that tibial plateau fractures and scaphoid fractures were the most frequently missed fractures, but this was not reflected in the data from 2014, perhaps suggesting that discrepancy meetings resulted in learning that may have reduced the incidence of tibial plateau and scaphoid fracture misses.
 Type of each discrepancy. All figures courtesy of Dr. Bhavna Batohi.
Type of each discrepancy. All figures courtesy of Dr. Bhavna Batohi.Also, 30 (63%) of misses were considered of low diagnostic difficulty, leading them to deduce that training strategies directed at commonly missed diagnoses may be valuable in significantly reducing errors. Now a summary of discrepancy meeting findings with examples of the commonest misses has been made available to all reporting radiologists, and a training module with a checklist system for wrist radiographs is being developed.
"Error is intrinsic in radiology. The daily error rate in radiology has been estimated to be between 3.5-4% and approximately 30% if considering only examinations which have confirmed abnormalities," noted lead author Dr. Bhavna Batohi in an e-poster presented at the 2015 congress of the European Society of Musculoskeletal Radiology (ESSR), held in York, U.K., in late June. "The cases presented to our discrepancy meetings are prone to selection bias and are not a true representation of the types of discrepancy or the error rate that occurs during day-to-day practice."
Regular discrepancy meetings are being implemented as part of quality assurance programs in radiology departments in the U.K., and the Royal College of Radiologists (RCR) has published standards outlining how to use the meetings as a tool for shared learning and to minimize patient harm. The purpose of the King's College audit was to detail some of the trends and highlight lessons learned during 2014 from MSK errors discussed at discrepancy meetings.
At King's, staff use an anonymous, form-based method to forward cases to the discrepancy meeting. Forms are collected by the meeting conductor and discussed with attendees following the monthly clinical governance meeting. The documents are analyzed to establish trends and collate key learning points to share with the department, Batohi and colleagues explained.
For each case, the imaging study type, study date, date of detection of the abnormality, and details of the discrepancy are recorded, and the diagnostic difficulty and potential clinical impact of the error is agreed at the discrepancy meeting. If one form highlights two investigations with errors identified, then this is analyzed as two separate cases. Similarly, if there is a study with two discrepancies identified, this is considered as two separate cases.
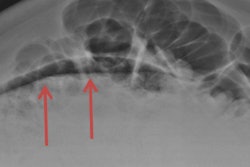
The time interval from when the error was made to when the discrepancy was identified ranged from zero to 363 days, with an average of 32 days and median of eight days. Almost all (47, 98%) MSK discrepancies were identified on plain radiography, apart from one case where spinal metastases were missed on a CT of the abdomen and pelvis. Where the discrepancy occurred on plain film and was not recognized on a subsequent plain film, the correct diagnosis was then made on MRI in 11 cases and on CT in five cases. Four out of the six triquetral fractures were identified subsequently on MRI.
 Classification of musculoskeletal discrepancies.
Classification of musculoskeletal discrepancies.The most common type of MSK error was a perceptual discrepancy (34, 71%), and 28 of these were missed fractures, four missed dislocations and three missed metastases. Three of these perceptual discrepancies were due to satisfaction of search and two due to the abnormality being outside the area of interest, or at the edge of the film, they stated.
There were nine cognitive discrepancies, including four overcalls, and one discrepancy due to lack of knowledge where the features of humeral head avascular necrosis were not recognized. Faulty reasoning accounted for four cognitive discrepancies:
- Lipohemarthrosis reported as an effusion
- Bilateral femoral avascular necrosis called degenerative change
- Subtalar dislocation was not recognized and only a displaced bone fragment recognized as being abnormal
- Triquetral fracture was called a lunate fracture.
Wrist fractures were the most commonly missed fractures (13/34), and of these there were six triquetral fractures and three distal radial fractures. Data from discrepancy meetings in 2013 showed that tibial plateau and scaphoid fractures were the most commonly missed, six and 10 cases respectively, but in 2014 these fell to zero and three respectively, according to the authors.
A total of 30 (63%) cases had a diagnostic difficulty scored as easy, and 27 (56%) had no or only a minor potential clinical effect of the patient. Four errors were considered serious or potentially fatal and these included a shoulder film and a humerus film where a humeral head metastasis was missed, a missed fractured scaphoid on a wrist film, and a missed thoracic spine metastasis on a thoracic spine film. All of these four discrepancies were given a diagnostic difficulty of moderate.
"Duty of Candour" legislation became active in the U.K. in late 2014, they pointed out. It imposes a legal duty on hospital, community, and mental health groups to inform and apologize to patients if there have been mistakes in their care that have led to significant harm, and aims to help patients receive accurate, truthful information from health providers. In the King's College audit, the authors considered that eight cases would have needed to invoke a Duty of Candour process.
"With the introduction of the Duty of Candour, a number of identified discrepancies may fall within the scope of legislation due to 'moderate harm' having occurred. Our discrepancy meeting forms have been modified to include this issue," Batohi et al concluded.