A group of experienced radiologists from Madrid has developed a comprehensive, practical approach to cut error rates, and they collected a certificate of merit at ECR 2017 in Vienna for their efforts.
To minimize errors, Dr. Paola Barón Ródiz and colleagues from the radiology department at Hospital Severo Ochoa in Madrid, recommended the following strategies:
- Adopt standardized and optimized imaging protocols.
- Recognize and correct imaging artifacts by developing a basic knowledge of CT and MR physics.
- Use appropriate and variable grayscale settings when evaluating CT studies so images have an appropriate contrast resolution to optimize the visualization of pathologic findings.
- Optimize working environment with respect to ergonomics and avoid interruptions, distractions, and glare affecting the monitor. Human factors such as excessive workload and fatigue should be avoided to maintain constant vigilance in interpretation of studies.
- Make a systematic search or a structured image evaluation. A well-designed checklist may urge radiologists to take a second look and to pay special attention to the first and last images in viewing series in cine mode to avoid "scrolling error."
- Review prior reports or imaging studies. Information from previous studies may improve accuracy and help to avoid significant errors. "Alliterative" or "satisfaction of report" errors occur more often when radiologists read the reports of previous examinations before looking at a new exam, so radiologists must perform their own interpretation before reading previous reports.
- Consult the literature when drawing conclusions about an unknown case to formulate a sufficiently broad range of differential diagnoses, and create a program of continuous learning to prevent knowledge gaps.
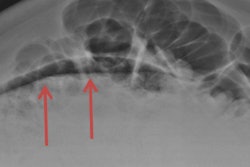
- Struggle to overcome cognitive biases and be familiar with causes of diagnostic pitfalls such as anatomic blind spots or normal anatomic variants to reduce a common cause of misinterpretation.
- Consult liberally with colleagues and/or referring physicians when a challenging case is encountered. Information obtained from these conversations often influences the final report and helps to avoid interpretative errors.
- Create multidisciplinary committees, particularly for cancer care. An important element here is the double reading of images that is made within the appropriate clinical scenario.
- Adopt communication protocols. Many errors are due to a poor communication at some stage in the imaging/reporting process. The adoption of a protocol for communication of urgent or unexpected radiological findings may reduce this type of error.
- Train radiologists to improve the clarity and effectiveness of their written reports so their message is not lost or misunderstood.
- Try to make double readings to safeguard the quality of the service, but this strategy implies a significant manpower issue for its routine adoption. Another option is to establish a peer-review program in which a percentage of studies are evaluated by colleagues to provide feedback about any diagnostic errors.
- Pay attention to individual physician factors such as illness or advancing age to ensure they do not significantly affect diagnostic performance.
- Use computer-assisted detection wherever possible. Several such systems are available, and although their clinical effectiveness remains controversial, this area holds much promise.
Pearls for head and neck imaging
In their e-poster at ECR 2017, the same authors also provided the following specific pearls to avoid diagnostic pitfalls in head and neck imaging:
- Nasopharyngeal cancer should be suspected in every adult who presents with an isolated otitis media with effusion.
- In the presence of otomastoiditis, look for its complications, especially in children.
- In the presence of sinusitis, look for its origin.
- Report the surgically risky anatomic variants.
- Remember that medication-related osteonecrosis of the jaw exists.
- In patients with chronic neck pain, look for rare causes such as calcification of the transverse ligament of the atlas or periodontoid pseudotumor.
- In patients with head and neck oncological history, look for perineural spread. Imaging plays a critical role because this condition may be asymptomatic and carries a grave prognosis. Furthermore, it is one of the most frequent missed diagnoses in head and neck imaging.
- If problems persist after correct treatment in head and neck cancers, look for adenopathies in anatomic blind spots such as retropharyngeal and retropectoral areas.
- Think outside of the box: Don't forget that parathyroid glands exist and they may be cystic or ectopic and may be located anywhere in their path of migration from the hyoid bone to the carina, or even inside the thyroid gland.
- Go back to basics: Look for intrathoracic goiters and possible tracheal compression. It may be basic, but it is frequently overlooked and it really matters to the patient and surgeon.
- Remember to evaluate head and neck muscle groups; findings may be surprising.
To view the authors' range of clinical cases presented at ECR 2017, click here.