CT is thriving, and instead of informing patients about the risk of radiation-induced cancer, now's the time to emphasize the upside of undergoing an examination, according to CT pioneer Willi Kalender, PhD. Tell them CT saves lives, he said in a special lecture at the U.K. Radiological Congress (UKRC) 2015.
"Keep in mind the benefits of CT are known and high. The risk of CT certainly is very low and very likely is zero," he noted. "The benefit-to-risk ratio has to be as high as reasonably achievable [AHARA]. Do not discuss risk with your patients, and stress AHARA instead of ALARA [as low as reasonably achievable]."
Huge progress in terms of dose reduction has occurred during the past two decades, and modern CT systems now operate at effective dose levels in the mSv and sub-mSv range, i.e., in the range of natural background radiation, noted Kalender, professor and chairman, Institute of Medical Physics at the University of Erlangen in Germany.
 Tell your patients CT saves lives, Willi Kalender, PhD, urged. Image courtesy of the European Society of Radiology.
Tell your patients CT saves lives, Willi Kalender, PhD, urged. Image courtesy of the European Society of Radiology.
"At the same time that we've seen all these improvements and dose has been cut by a factor of five, it's rather disturbing that some 'experts' and media like to come up with horror stories," he told delegates in a plenary lecture at the UKRC 2015. "Whereas in the 1990s it was said 'CT is dead,' now they say 'CT is deadly'... that's sheer nonsense to me!"
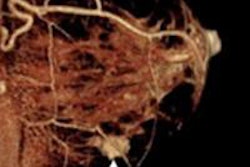
Intelligent approaches and innovative technology now exist, continued Kalender, who is a consultant for Siemens Healthcare . For instance, Dr. Stefan Schoenberg from the University of Mannheim in Germany, recently described a cardiac exam with an effective dose of 0.22 mSv and 70 cm/sec table feed, 0.3 sec scan time, 70 kV with tube current modulation, dynamic collimation, iterative reconstruction, and dose-efficient "low-noise" detector.
The risk estimate for a 0.22 mSv CT scan is virtually nil, Kalender noted. Assuming the worst case scenario of a 5% mortality per 1 Sv effective dose, which is valid for the high-dose range and also holds true for the low-dose range, this would mean five patients out of 100 exposed to 1 Sv (high dose), five patients out of 100,000 exposed to 1 mSv, or one patient out of 100,000 exposed to 0.2 mSv is at risk of dying from x-ray induced cancer. Risks of between 1:100,000 and 1:10,000 are described as very low, he said.
Choosing the right CT unit
Kalender warns against automatically selecting a CT scanner with the largest number of detectors, even though some companies promote them aggressively.
"You don't always buy the fastest car with the most horsepower value because you may not be able to make any use of it," he said. "With the detectors, it is very difficult because the larger the field is, the more scattered radiation you will have, and there are other more subtle effects."
In 2008, 320 x 0.5 mm detectors with a rotation time of 0.35 sec were introduced, and the next innovation on the horizon is likely to be 2,048 x 0.4 mm detectors taking 0.2 sec. However, the height and size of the detector are the really important aspects, not the number of rows, insisted Kalender, who recently obtained promising results from a new 512-row detector with a height of only 5 cm.
| State of the art in multislice spiral CT | |
| Rotation time per 360° | 0.27-0.35 sec |
| Slice width | 0.5-0.6 mm |
| Simultaneously scanned slices | 64 (-320) |
| Z-coverage per rotation | 40-160 mm |
| Scan times "whole body" | <1-20 sec |
| Scan range | >1,000 mm |
| Isotropic spatial resolution | 0.4-0.6 mm |
| Effective dose | <1-10 mSv |
Slice width is another vital consideration, and he emphasized the importance of not only spatial resolution in-plane but also cross-plane, for which thin slices are necessary. As for scan times, whole-body exams in infants can be performed in less than a second, and there may be scope for even more improvement. Scan ranges are virtually unlimited now, and more important factors are isotropic spatial resolution and effective dose, Kalender noted.
The demands on today's scanners are such that their mechanical design has to withstand very fast rotations, and centrifugal forces acting on the x-ray tube can be 30 g or more. To take account of higher speeds, x-ray power must increase, and image acquisition of up to 2 x 120 kW is now achievable for dual-source CT units. For cardiac CT, combining the data from a dual-source examination can be a particular advantage, and a quarter rotation may be sufficient, e.g., 65 ms temporal resolution (trot/4), he explained.
Overall, effective scan times of below 0.1 sec are available and reducing rotation further is feasible, but it's unclear whether there is an obvious need for acceleration, according to Kalender.
Increasing high-contrast spatial resolution is primarily about x-ray detectors, tubes, and algorithms. Most state-of-the-art detectors use scintillators, reflectors, and 3D antiscatter grids, which is fine for image quality, but the major weakness is the geometric efficiency. Geometric efficiency can be as low as 70%, and this is an area on which the Erlangen group is working at present. The resolution depends on detector pixel size and affects image pixel noise very strongly, and in 3D CT with isotropic spatial resolution, pixel noise standard deviation and thereby dose go with the fourth power of the resolution element, he added.
"Improvements of spatial resolution are possible but may be in conflict with other parameters, above all with limiting dose. Further improvements of low-contrast soft-tissue visibility are likely due to many advances and optimization steps," Kalender said, noting that algorithms like model-based iterative reconstruction are important here.
Dedicated scanners
CT of the peripheral anatomy is showing promise, even though the technology is not yet mature. Flat-detector (FD) CT systems are of interest for dedicated applications such as dentomaxillofacial exams, breast CT, and small-animal imaging with micro-CT. An example of modern FDCT systems for orthopedic extremity imaging is the Verity flexible system from Medplan Oy in Finland.
Small, dedicated CT scanners primarily focusing on maxillofacial and ear, nose, and throat applications have swamped the market, he said. Getting reliable recent figures is hard, but Germany has more than 1,000 dental cone beam CT and digital volume tomography systems, while the U.S. has more than 3,000 systems. Manufacturers claim these systems provide higher spatial resolution and lower dose, but they avoid standard CT testing and regulations.
"For once, I think more regulations would be OK in this case," Kalender said.
He also said the breast CT scanner with a cadmium telluride (CdTe) detector unveiled at RSNA 2014 by CT Imaging (a company founded by Kalender) is progressing well. The first clinical feasibility studies are planned for the final quarter of 2015 in Erlangen and Aachen, and will be supported by the German Federal Ministry of Education and Research (Bundesministerium für Bildung und Forschung, BMBF). He is convinced his new scanner (133 CT slices, 0.15 mm thickness) compares very favorably with tomosynthesis (56 tomo slices, thickness not specified) and mammography (projection image, 20 mm thickness).
Overall, CT is certainly alive and well, he concluded. A large variety of CT scanners is emerging, and higher resolution and lower dose levels are expected. Radiologists must stress the benefits of CT, not the low, very hypothetical risks. Tell your patients CT saves lives, he recommended.