Compelling new evidence of postmortem MRI's value has emerged. It can provide clinically important information in more than half of cases in which a conventional autopsy is nondiagnostic, typically in fetuses, according to a recent U.K. study.
The large, double-blinded prospective study compared conventional autopsy with the diagnostic accuracy of noninvasive, cerebral postmortem MRI, specifically for cerebral and neurological abnormalities in fetuses and children. The research team found postmortem MRI is accurate for identifying significant neuropathology in fetuses and children, and it may provide vital information even in cases in which formal neuropathological examination cannot occur (Clinical Radiology, 4 June 2015).
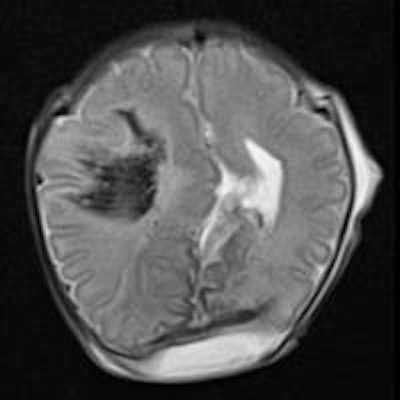
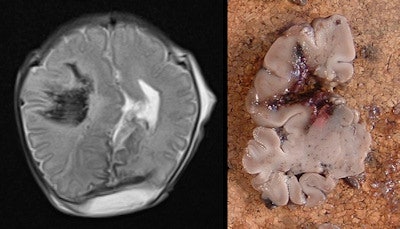 Example of intracranial hemorrhage. Axial T2-weighted postmortem MRI demonstrates right frontoparietal parenchymal hemorrhage in a 35-week gestation, fetal stillbirth (left), confirmed on histology (right). All images courtesy of Dr. Owen Arthurs.
Example of intracranial hemorrhage. Axial T2-weighted postmortem MRI demonstrates right frontoparietal parenchymal hemorrhage in a 35-week gestation, fetal stillbirth (left), confirmed on histology (right). All images courtesy of Dr. Owen Arthurs.Studies such as this are changing the way autopsies are performed and helping to develop the concept of less-invasive autopsy, according to lead study author Dr. Owen Arthurs, a National Institute for Health Research clinician scientist and academic pediatric radiologist working at Great Ormond Street Hospital for Children and University College London (UCL) Institute of Child Health.
"Less-invasive autopsy involves postmortem imaging and ancillary tests, with or without tissue biopsy," he wrote in an email to AuntMinnieEurope.com. "Because many parents do not agree to a traditional full autopsy, less-invasive approaches have significant implications for future clinical practice. They can provide additional diagnostic information for more families and also information for public health and governance, where data are currently missing in many cases."
Because postmortem MRI has high accuracy in detecting congenital abnormalities and other major brain pathology in fetuses and children, it may be used as a screening tool for detecting significant brain abnormality, noted the Magnetic Resonance Imaging Autopsy Study (MaRIAS) group, which is led by Dr. Andrew Taylor, professor of pediatric cardiac radiology, and Dr. Neil Sebire, professor of pediatric pathology, both from UCL.
"This may be useful in identifying those cases in whom neuropathological examination would be appropriate, and confirm suspected cases of antenatally detected brain malformations and major intracranial bleeds, for parents in whom standard autopsy is unacceptable," they added.
How postmortem MRI compares
Conventional autopsy has been regarded as the reference standard for postmortem investigation to determine the cause of fetal and pediatric deaths and also to investigate relevant pathologies. However, conventional fetal autopsy with formal neuropathological examination may be challenging for several reasons.
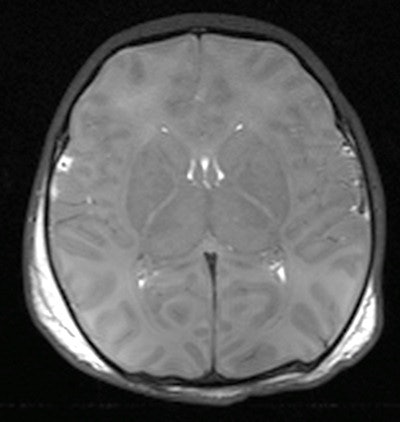 Axial T2-weighted postmortem MRI demonstrates hypoxic injury to the brain, with poor gray-white matter differentiation and cerebral edema. Differentiating antemortem from postmortem hypoxia is difficult on conventional postmortem MRI sequences.
Axial T2-weighted postmortem MRI demonstrates hypoxic injury to the brain, with poor gray-white matter differentiation and cerebral edema. Differentiating antemortem from postmortem hypoxia is difficult on conventional postmortem MRI sequences.For one, the fetal and neonatal brain is relatively poorly myelinated with greater water content, and, thus, is friable and requires prolonged fixation in formalin prior to sectioning (which may take up to three weeks) causing a delay for funeral proceedings. Also, changes following death or maceration and cell breakdown may render histopathological examination uninformative. And in some situations, detailed examination of the intricate connections and anatomical structure of the brain and spinal cord is best done with the brain in situ, particularly for posterior fossa lesions.
MRI is a particularly good, noninvasive, high spatial resolution exam that gives excellent image contrast between cerebrospinal fluid and brain tissue, thus providing distinct anatomical details. Postmortem MRI, when used in conjunction with other ancillary investigations, has recently been shown to have a high diagnostic accuracy rate for cause of death or main diagnosis compared with traditional autopsy in fetuses, stillbirths, and children.
Most research, however, has focused on an unselected population for the major diagnosis or cause of death without a detailed analysis of neurological abnormalities -- until now.
The researchers of the current study performed preautopsy cerebral postmortem MRI in a sequential, prospective cohort of 400 fetuses and 123 children younger than 16 years of age. Postmortem MRI and conventional autopsy findings were reported blinded and independently of each other.
| Cerebral postmortem MRI results | ||
| Findings | Sensitivity | Specificity |
| Cerebral malformations | 88.4% | 95.2% |
| Major intracranial bleeds | 100% | 99.1% |
| Overall brain pathology | 87.5% | 74.1% |
Formal neuropathological examination was nondiagnostic due to maceration/cell breakdown in 16% of fetuses; of these, cerebral postmortem MRI provided clinically important information in 53%. The sensitivity of postmortem MRI for detecting significant antemortem ischemic injury was only 68% overall.
The negative predictive value was 92.2% for overall significant brain injury, implying opening the skull at autopsy to fix and examine the brain histologically is unlikely to detect a neurological cause of death in which the clinical history is nonsuggestive and the postmortem is normal, they added.
"Previous postmortem studies by several groups have all shown good agreement between central nervous system abnormalities at autopsy and [postmortem MRI]," the researchers wrote. "However most of these studies were small and retrospective, without adequate masking of imaging and autopsy data, and mainly involved fetuses; there are limited data on newborns and children. Autolysis or maceration, recognized as a cause of noncontributory autopsy findings, also affects the quality of [postmortem MRI]; however, [postmortem MRI] may be still useful and provide clinically important information in these cases, even when neuropathological examination is nondiagnostic."
They go on to write that routine use of postmortem MRI prior to fetal brain autopsy may significantly reduce the nondetection rate for clinically significant pathologies that are difficult to assess, such as posterior fossa malformations.
"In fetuses and stillbirths, cerebral [postmortem MRI] should be performed routinely if there is suspected cerebral pathology, even when consent has been obtained for conventional neuropathological examination, as such data may direct the conduct and reporting of the autopsy and may provide additional clinical information," they wrote.
Limitations
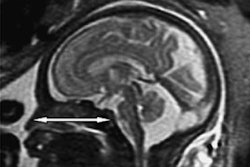
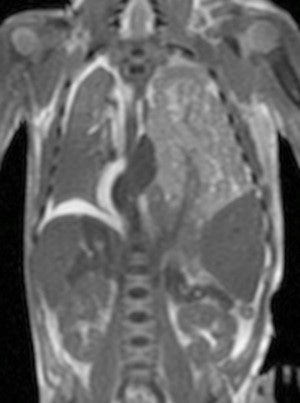 Postmortem MRI is widely used for non-neurological conditions. Coronal T2-weighted postmortem MRI of a term stillbirth with large left-sided congenital diaphragmatic hernia, containing predominantly small bowel.
Postmortem MRI is widely used for non-neurological conditions. Coronal T2-weighted postmortem MRI of a term stillbirth with large left-sided congenital diaphragmatic hernia, containing predominantly small bowel.The researchers are quick to point out that postmortem MRI is currently less reliable for detecting hypoxic ischemic injury, with both false-positive and false-negative results.
Also, these cases were all interpreted by specialist pediatric radiologists in a tertiary center, so may not represent what could be offered in other institutions. It is also difficult to interpret cases correctly as most errors were interpretative and not observational. This emphasizes the need for specialist education in the field to maximize the diagnostic yield from both imaging and autopsy.
Lastly, the researchers acknowledge that specific details of congenital brain malformations were not assessed in the study beyond the category of abnormality; for example, postmortem MRI may be accurate for detecting lissencephaly, but is unlikely to provide detailed information regarding subtyping or other histological-based features.
Future plans
The researchers are continuing to develop novel imaging and autopsy methods to offer the best possible less-invasive autopsy to bereaved parents who do not wish to have a full, invasive autopsy, according to Arthurs.
Their current research is focusing on more advanced diagnostic postmortem MR methods such as diffusion-weighted imaging (DWI) for forensic postmortem interval-based research and novel methods of tissue sampling.
Arthurs recently established the Paediatric Working Group of the International Society Forensic Radiology and Imaging and also the Postmortem Imaging Taskforce of the European Society of Paediatric Radiology to deal with getting international consensus on the approaches to postmortem imaging.