MRI is as accurate as autopsy in demonstrating macroscopic details of brain abnormalities and postmortem MRI may represent a valuable extra tool in cases in which autopsy cannot be performed, according to award-winning Spanish research.
"MRI provides useful morphologic information of the CNS (central nervous system) in dead fetuses. We found a close correlation between MRI structural findings and autopsy," noted Dr. Laura Oleaga, a radiologist at the Hospital Clinic in Barcelona, and her colleagues. "The role of MRI is not only limited to detection of major pathology; other pathological lesions detected might have an important part in advancing of medical research and knowledge."
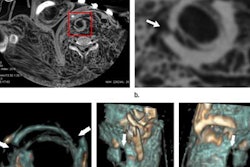
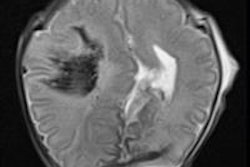
Oleaga et al shared their experiences in an e-poster that won a prestigious cum laude award at RSNA 2014.In the fetuses they have studied over the past two years, MRI depicted the brain limits and residual brain tissue well in one case of hydranencephaly. In a case of aqueductal stenosis evaluated with intrauterine ultrasound, MRI demonstrated the dysplastic mesencephalon and guided the autopsy evaluation. In cases of cytomegalovirus infection (CMV) infection, the subependymal cysts were depicted well on MRI.
The authors' goals were to review the postmortem MRI protocols in the evaluation of fetuses and stillborn neonates, to learn the normal CNS findings related to the postmortem status, and to correlate the MRI findings in CNS diseases with intrauterine sonography and histopathology.
Perinatal losses are common in routine obstetric practice, complicating about 1% to 3% of pregnancies, they reported. This may be due to unexplained intrauterine deaths, or caused by fetal abnormalities or maternal disease.
"It is important to know the cause of death for parents' counseling," Oleaga and her colleagues stated. "Invasive autopsy is at present the gold standard to evaluate the fetuses. In 30% of cases, invasive autopsy can provide important additional information that was not available prenatally."
However, conventional autopsies have some limitations in cases of small fetuses, and depending on the length of time between death and autopsy, autolysis (especially of the brain) does not supply adequate information. Furthermore, there are major practical problems associated in performing autopsy on CNS structures without formalin fixation, and the fetal or stillborn brain is difficult to handle even with adequate fixation.
"Many parents would like to know the cause of the demise and if there is an increased risk of abnormalities in future pregnancies," the authors wrote. "But parents frequently request that all organs must be replaced before burial, which makes adequate fixation impossible, or in certain cases refuse autopsy. Imaging has been used in the study of postmortem abnormalities of fetuses and neonates, but this has been limited to conventional radiology, usually to assess the chest or bones."
In February 2012, the Barcelona team started performing postmortem MRI studies in deceased and stillborn fetuses in cases of parent refusal to allow a conventional autopsy, or as an adjunct to autopsy. They showed the normal findings in CNS after demise due to the postmortem status, and presented the MRI findings in a variety of pathological CNS processes with intrauterine sonography and histopathological correlation.
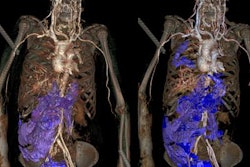
Scans were done between one and three days after death. The studies were performed on 1.5- and 3-tesla units, using an eight-channel phased-array head coil, along with sagittal 3D T1-weighted (MPRAGE), sagittal 3D T2-weighted, axial 3D T2-weighted constructive interference steady-state (CISS), axial diffusion-weighted, and axial susceptibility-weighted imaging (SWI) sequences.
| Protocol at 1.5 tesla | |||||
| 3D sagittal T1W | 3D sagittal T2W | 3D axial CISS | ep2d_diff_800 | SWI | |
| Repetition time (TR) | 1850 msec | 2700 msec | 6.46 msec | 10100 msec | 27 msec |
| Echo time (TE) | 4.56 msec | 381 msec | 2.44 msec | 185 msec | 20 msec |
| FA | 8° | 120° | 60° | 90° | 15° |
| Field-of-view (FOV) | 120 mm | 120 mm | 120 mm | 120 mm | 120 mm |
| Matrix | 256 x 256 | 256 x 256 | 512 x 512 | 192 x 256 | 192 x 256 |
| Thickness | 0.8 mm | 1 mm | 0.5 mm | 3 mm | 1 mm |
| Protocol at 3 tesla | |||||
| 3D sagittal T1W | 3D sagittal T2W | 3D axial CISS | ep2d_diff_800 | SWI | |
| TR | 1710 msec | 3200 msec | 6.8 msec | 11000 msec | 28 msec |
| TE | 2.65 msec | 394 msec | 2.95 msec | 163 msec | 20 msec |
| FA | 8° | 120° | 50° | 90° | 15° |
| FOV | 110 mm | 110 mm | 110 mm | 110 mm | 110 mm |
| Matrix | 256 x 256 | 384 x 384 | 512 x 512 | 192 x 256 | 192 x 256 |
| Thickness | 0.8 mm | 0.5 mm | 0.3 mm | 2 mm | 0.57 mm |
If appropriate, fresh tissue samples were taken for polymerase chain reaction (PCR)-based microbiologic assays. Brain, brainstem, and cerebellum were extracted "in toto" and fixed for three weeks in 4% formaldehyde with 10% acetic acid solution. Neuropathological analysis was conducted through frontal serial sectioning at 1 cm to 2 cm intervals. After careful inspection, sampling for histological examination was performed, and the slides were stained with hematoxylin and eosin. Immunohistochemistry was applied if necessary.
Their study was based on cases of spontaneous intrauterine demise, death of premature newborns, and elective termination of pregnancy. The gestational age ranged between 21 weeks to 41 weeks (average 31.7 weeks). In a total of 23 cases, 15 postmortem MR examinations were performed on a 3-tesla system, the remaining eight being carried out on a 1.5-tesla unit. Intrauterine ultrasound was performed in all cases, and 17 conventional autopsies and two intrauterine MR examinations were undertaken. There were six cases of ventriculomegaly, five of periventricular cysts, two of migration abnormalities, and one case each of hydraencephaly, DNET, periventricular leucopathy, and brain hemorrhage.
They described a case of a 24.3-week elective termination of pregnancy due to cytomegalovirus infection. Intrauterine ultrasound demonstrated bilateral ventricular dilation and periventricular hyperechogenicity, and intrauterine MRI showed bilateral ventriculomegaly. Postmortem MRI highlighted the ventricular dilation and periventricular cysts, and pathology demonstrated the ventricular dilation, although macroscopic pathology did not demonstrate the subependymal cysts. Ventriculitis and periventriculitis with disruption of the ependymal lining were identified.