
Global researchers who are eager to gain experience in fetal autopsies using CT and MRI are facing immense frustration due to ongoing difficulties over obtaining consent, and one investigator reports being "hamstrung" by the procedures and bureaucracy of ethics committees.
New data presented at last month's Combined Scientific Meeting (CSM) in Melbourne, Australia, showed that fetal CT scanning can be a useful adjunct to conventional autopsy. In cases where fetal autopsy is not appropriate, fetal CT can still provide useful additional information to assist with parent counseling, according to lead author Dr. Sarah Constantine, a dental and general radiologist at the Queen Elizabeth Hospital and the Women's and Children's Hospital in Adelaide, South Australia.
"In a busy hospital with very distraught parents, getting a separate consent is not easy," she noted in an email to AuntMinnieEurope.com. "We are continuing to try and recruit new cases, but it took a long time to get the few we wrote about, as ethics [committees] have hamstrung us by insisting on a separate consent form for the study. Our current autopsy consent form includes a section on research, but the ethics committee felt this was not enough, so we have a separate form."
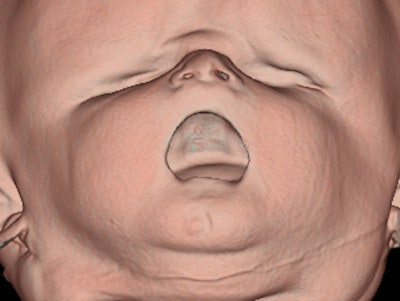 Surface-rendered CT image of a 38-week-fetus shows the intact palate. All images courtesy of Dr. Sarah Constantine.
Surface-rendered CT image of a 38-week-fetus shows the intact palate. All images courtesy of Dr. Sarah Constantine.Constantine and her colleagues plan to approach the local ethics committee again soon with their interim findings to see if they can persuade them to let them use a single consent form because this would give access to around three or four fetuses per week on average. They are also looking at the possibility of injecting diluted contrast into the fetal heart under ultrasound guidance to improve visualization of the heart.
Unexplained stillbirths account for more than 25% of all fetal deaths, and have multiple causes, she explained. In at least a third of cases, autopsy can provide important information about the pregnancy that was not available antenatally, but often doctors are reluctant to ask for consent and some grieving parents are unable to consent for a variety of reasons. This leaves many parents at a clear disadvantage when being counseled for future pregnancies, which previously could not be avoided, noted Constantine et al in their CSM 2014 e-poster.
"While our preliminary scans did not detect all fetal abnormalities, some valuable information was obtained, and there are some features such as bony abnormalities, which can be difficult to elucidate at autopsy," they wrote.
CT scanning is best performed as soon as possible after arrival to maximize tissue contrast, and does not significantly delay funeral/burial preparations, according to the authors. The potential use of intravenous contrast may also assist in providing further diagnostic information, and dual-energy multidetector CT (MDCT) may be useful in pregnancy losses where conventional autopsy is not appropriate.
MRI is useful in the investigation of fetal abnormalities, particularly in the examination of the neural axis and soft tissues, and virtual MR autopsies are accepted by almost all parents, compared with an acceptance rate of around two-thirds for conventional autopsies, they continued. Much depends on the mother's religious background, and Muslim parents tend to be far less likely to consent to a conventional autopsy. However, the availability of MRI is limited, and a comprehensive examination with MRI is time-consuming. Because MRI signal relies upon the movement of free hydrogen atoms, signal quality is reduced in the postmortem patient due to cooling and/or refrigeration.
In contrast, all but the most remote communities have access to CT scanners, and the relative speed with which a scan can be performed allows scanning quickly after arrival. Furthermore, body temperature is not important, allowing CT scanning to be performed at any stage after fetal demise.
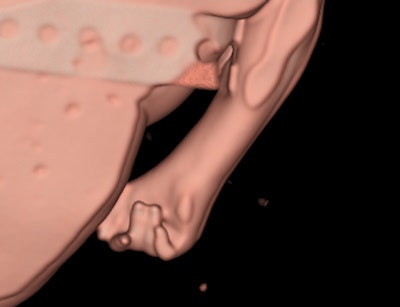 Surface-rendered CT image of a 20-week-fetal hand demonstrates the typical overlapping digits of trisomy 18.
Surface-rendered CT image of a 20-week-fetal hand demonstrates the typical overlapping digits of trisomy 18.Constantine and her colleagues investigated the value of dual-energy MDCT as part of the inquiry into fetal abnormalities and pregnancy losses in the second and third trimesters, and early neonatal period. The study was approved by the Women's and Children's Hospital Network Human Research Ethics Committee. Patients were recruited while giving consent for conventional autopsy.
The fetuses were scanned as they arrived in the department of surgical pathology, wrapped in surgical drapes, and were not repositioned for the scan. To maximize contrast resolution, each fetus was imaged twice using a single-source spectral dual energy CT unit.
Firstly, a high-definition helical scan was completed permitting the maximum spatial resolution possible for multiplanar bone and 3D volume rendered skeletal imaging (3D skeleton). This was followed by a dual energy acquisition. Both high and low energy (kVp) datasets were acquired simultaneously for near perfect anatomical registration.
The dual energy image set was evaluated for the optimal image contrast and image noise. The optimal monochromatic energy level (keV) was concluded and a new image set was created for multiplanar evaluation of soft-tissue organs.
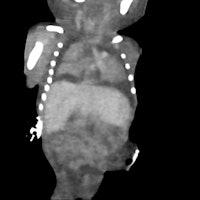
 3D skeletal reconstruction shows a hemivertebra and extra rib.
3D skeletal reconstruction shows a hemivertebra and extra rib.A conventional autopsy was performed on each fetus after CT scanning by an experienced pediatric/neonatal pathologist. The CT scans were analyzed by a perinatal radiologist (Constantine herself), together with a pediatric/neonatal pathologist (co-author Dr. Lynette Moore, an associate professor).
The clinical details (except gestational age) were withheld. The fetal biometry as well as findings relating to an external examination and internal organs were measured and recorded. The CT findings were then compared with the autopsy result, which was considered the gold standard.
Six fetuses were initially scanned. Three fetuses had been delivered after death in utero, and three were from pregnancies terminated due to fetal abnormalities. In all but one fetus, the crown-rump and crown-heel length measurements determined on CT were within 6% of the autopsy measurements. There was quite poor correlation between CT and autopsy measurements of the fetal foot length and head measurements, probably due to fetal positioning; the foot can be more easily "straightened" during a direct examination.
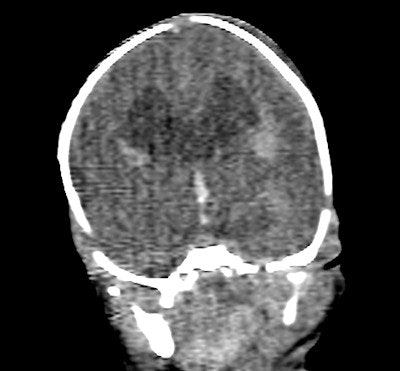 Coronal image of the brain shows dilated cerebral ventricles.
Coronal image of the brain shows dilated cerebral ventricles.Evaluation of the heart was poor on CT, as was expected in a noncontrast postmortem study, the authors reported. The heart was correctly identified as normal in fetus 5, but much of the heart could not be commented upon, and even the great vessels were difficult to confidently identify. Significant cardiac abnormalities were identified in fetuses 2 and 3 at autopsy. The diaphragm could be seen to be intact in four of the fetuses at CT, and was intact in all fetuses at autopsy.
The liver and spleen were identified in the correct position in four fetuses, and were not able to be assessed in two fetuses on CT. The kidneys proved very difficult to identify due to the absence of intra-abdominal fat. In the three fetuses that were identified on CT, the kidneys were normal at autopsy. The kidneys were not identified in fetus 4 on scanning, and at autopsy the renal parenchyma was multicystic dysplastic in nature and horseshoe in morphology. The gallbladder and pancreas were not reliably seen in any fetus on CT.
Scott Brown, head radiographer for CT at the Women's and Children's Hospital in Adelaide, was the third author of the CSM e-poster.
Meanwhile, in an open access article posted online by European Radiology on 31 August, U.K. authors led by Owen J. Arthurs from London's Great Ormond Street Hospital for Children National Health Service (NHS) Foundation Trust have published their findings on the diagnostic accuracy of postmortem MRI for thoracic abnormalities in fetuses and children.
Having obtained institutional ethics approval and parental consent, they performed postmortem MRI on 400 unselected fetuses and children before conventional autopsy (Eur Radiol. November 2014, Vol. 24:11, pp. 2876-2884).



















