PET and MRI each bring advantages for imaging myocardial infarction (MI) and gauging myocardial viability. So it makes sense to do them both in a single exam, concludes a study of 25 MI patients presented last week at the European Society of Cardiology (ESC) congress in Barcelona, Spain.
In their study of 25 patients with a wide range of myocardial infarction types, imaging with PET/MRI found significant correlation between the PET part of the exam and late gadolinium enhancement (LGE) MRI scans, as long as the infarction was large enough to be transmural, the investigators found. PET routinely showed larger regions of ischemia than late gadolinium enhancement at MRI, potentially highlighting myocardial tissue at risk that could be protected using the right techniques.
Routine use of the hybrid modality could potentially improve risk stratification in patients with acute ischemia, the group from University Hospital Essen in Germany reported.
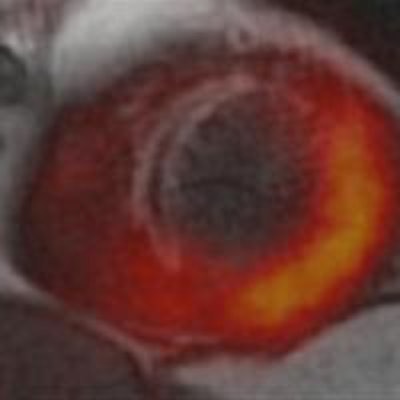
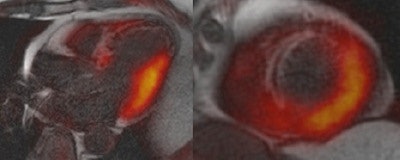 Fusion image of LGE MRI and PET in a four-chamber long-axis (left panel) view and a short-axis view (right panel) in a 60-year-old man with ST segment elevation myocardial infarction (STEMI) because of a proximal occlusion of the left anterior descending (LAD) artery. MRI revealed a transmural infarction within nearly the entire septum and the apex of the left ventricle (late gadolinium enhancement with an area of no-reflow), whereas a corresponding area of reduced tracer uptake can be seen in the perfusion territory of the LAD. The fusion images also demonstrate a significantly larger defect of FDG uptake (reduced viability) than the extent of the late gadolinium enhancement image. All images courtesy of Dr. Ercan Tezgah.
Fusion image of LGE MRI and PET in a four-chamber long-axis (left panel) view and a short-axis view (right panel) in a 60-year-old man with ST segment elevation myocardial infarction (STEMI) because of a proximal occlusion of the left anterior descending (LAD) artery. MRI revealed a transmural infarction within nearly the entire septum and the apex of the left ventricle (late gadolinium enhancement with an area of no-reflow), whereas a corresponding area of reduced tracer uptake can be seen in the perfusion territory of the LAD. The fusion images also demonstrate a significantly larger defect of FDG uptake (reduced viability) than the extent of the late gadolinium enhancement image. All images courtesy of Dr. Ercan Tezgah."We think you should combine PET and MRI because MRI shows really the infarction but PET might show us the ischemic zone of the myocardium, which is not really infarcted now," said cardiologist and lead author Dr. Ercan Tezgah in an interview with AuntMinnieEurope.com.
"When you do both PET and MRI, PET can show us the infarction with late gadolinium enhancement where PET might show us the ischemic zone of the myocardium, which is the area at risk that is not really infarcted." Therefore, both imaging modalities can show something about salvageable myocardium, he said.
Tezgah, along with radiologist Dr. Felix Nensa and colleagues, performed simultaneous PET/MRI in 25 prospectively enrolled patients with acute myocardial infarction (n = 19 with ST elevation or STEMI, n = 5 without or NSTEMI), as well as early percutaneous coronary intervention.
The researchers looked for regional wall motion abnormalities (WMA) from cine sequences on MRI, and compared them with FDG uptake in each myocardial segment, Tezgah explained.
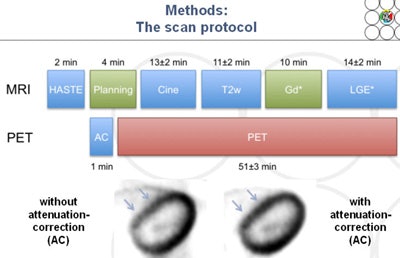
MRI was performed on a 3-tesla PET/MRI scanner (Biograph MMR, Siemens Healthcare). PET was performed on the same system with a field-of-view of 26 cm.
The researchers analyzed the hybrid images and measured them in several ways:
- The area of enhancement on late gadolinium enhancement images as a percentage of the total area (LGE %)
- The area of reduced FDG uptake (PET %)
- The extent to which PET/MRI correlated with enzyme and angiography findings regarding infarct size with respect to infarct transmurality (ITM)
Overall, PET % correlated significantly with LGE % (r = 0.57, p < 0.01) and ITM (r = 0.44, p = 0.028), the study team reported.
In 24 of 25 patients (96%), PET % (31 ± 11%) was even larger than LGE % (10 ± 10%) -- a difference that was highly significant (p < 0.0001).
And as stated, almost a quarter of the patients (6/25, 24%), the myocardial infarction was confirmed by reduced glucose metabolism as shown in PET % (32 ± 5%), even though no LGE was detectable at MRI, the investigators found.
Importantly, the correlation between PET % and LGE % depended on infarct transmurality, Tezgah said. With ITM of less than 50%, ITM correlation between the two modalities was weak (r = -0.19, p = 0.50), but it grew stronger with ITM of 50% to 75% (r = 0.68, p = 0.14), and stronger still with ITM of 75% or greater (r = 0.99, p = 0.01).
"Correlation was better with bigger infarcts than in patients with less transmurality," Tezgah said. The larger infarct area in PET images might represent tissue that might be at risk but isn't infarcted, at least not yet.
To look further into the differences between the two modalities, the group went on to compare the findings with troponin I elevation, which denotes myocardial tissue necrosis, and ST elevation. As expected, troponin I levels correlated well with LGE but not with PET in the majority of cases where PET showed a larger infarct. ST elevation was not a factor in any results.
"We saw that PET imaging might show another aspect of MI, maybe the boundary region," Tezgah said.
The group has already begun follow-up studies to determine precisely what is happening when different regions are highlighted.
"You can do both modalities in two examinations, of course, but we think the power of MRI was in higher temporal resolution, higher spatial resolution with its ability to show morphology and function," he said. "PET is the gold standard for showing viability, so it's the full power of noninvasive imaging in one examination and there's no time delay, so we see the best results when you do one examination."
The original 25 patients have been followed up at six, nine, and 12 months, and another 35 or so new patients have been scanned, Tezgah said.
The hybrid exam is equally accurate in patients with and without ST elevation. No differences were found between these groups, between men and women, nor for any clinical characteristics, Tezgah said. Imaging did show different things in different patients, and additional studies are underway to further probe any differences in study results.
New studies in larger cohorts may also reveal more possibilities of the hybrid exam, like showing postinfarct inflammation, and varying the amount of FDG could also open up new possibilities, for example reducing the influence of infarct transmurality on the correlation of results, Tezgah said.
Simultaneous assessment of myocardial injury by hybrid PET/MRI in patients with acute myocardial infarction showed high conformity between PET and LGE images, depending on ischemic transmurality. It may improve risk stratification of patients in the setting of acute ischemia, and hybrid imaging with PET/MRI may improve discrimination of the ischemic area and the already infarcted area of the myocardium, the authors reported.
PET/MRI could also lead the way toward salvaging more myocardial tissue at risk, he said.
In any case, Tezgah said, the interdisciplinary teamwork at University Hospital of Essen is well suited to teasing out the best results.
"We collaborate with all the disciplines, with cardiology, with radiology, and pathophysiology, and nuclear medicine. We discuss all of our findings and our knowledge," he said. "Radiologists are the best for image analysis, while the cardiologists provide knowledge about the clinical findings, and pathophysiology is very important to understand what we find."