In radiographic examinations, the standing weight-bearing position can be of crucial importance for the patellar position in the trochlear groove and for visualization of osteoarthritis in the medial patellofemoral (PF) joint, Danish researchers have found.
"The present technique for standing axial radiographs rarely allows weight bearing with both the hip and the ankle aligned vertically," noted Nikolaj Skou, a resident in the department of radiology at Aarhus University Hospital. "Medial patellar tilt and displacement relative to the femoral trochlea on axial PF radiographs may be an obligatory biomechanical effect of weight bearing."
 The city of Riga in Latvia provided a spectacular backdrop for the annual meeting of the European Society of Musculoskeletal Radiology (ESSR) in late June.
The city of Riga in Latvia provided a spectacular backdrop for the annual meeting of the European Society of Musculoskeletal Radiology (ESSR) in late June.In an e-poster that received one of the three winners' awards presented at the annual meeting of the European Society of Musculoskeletal Radiology (ESSR) held in Riga, Latvia, at the end of June, he explained that PF pain syndrome is thought to be associated with mechanical factors. Neither CT nor MRI has contributed significantly to determine the causal pathway or treatment, and based on clinical examination and imaging in the supine position, patellar maltracking with lateral displacement is still believed to be a leading cause of PF pain.
Axial radiographs of the PF joint in the supine position have demonstrated lateral PF osteoarthritis (OA) more commonly than medial PF-OA, but medial PF-OA appears to be as prevalent as lateral OA by standing axial radiographs of the PF joint and in large studies using MRI, according to Skou and his co-author Dr. Niels Egund, former president of the Scandinavian Society of Radiology.
Study details
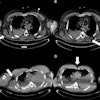
The two researchers compared patellar position in the trochlear groove and assessed the detection of medial and lateral PF joint space narrowing on axial radiographs in both a supine and standing position. Their study sample constituted 36 women and 23 men with a mean/median age of 56/57 (18-87 years). Six patients had a scan of of one knee only, resulting in a total of 112 knee examinations.
Standing weight-bearing axial radiographs of the PF joint in 30° knee flexion with weight bearing on one leg were obtained using a support device that kept the lower leg in 15° inclination. Axial views of the PF joint in the supine position were obtained in 30° knee flexion.
To position the patient for the axial standing radiographic view of the right PF joint, the inclination of the lower leg at 15° was secured by a device supporting the knee and lower leg. In this position, most tibial plateaus and patellar articular surfaces are in alignment with horizontal and vertical beam directions respectively, and the computed radiography (CR) detector plate is placed corresponding to the central beam. Weight bearing is primarily on the right leg using the left leg for slight support only, and the weight bearing axis from the hip is dorsal to the ankle.
When performing the axial radiographic view of the PF joint in the supine position, the angle between the central beam and the ventral aspect of the lower leg should optimally be less than 15° and the film cassette or CR detector plate perpendicular to the central beam, the authors wrote.
These workstation measurements on supine and standing axial PF radiographs were made: differences in patellar tilt, medial/lateral patellar displacement, and differences in medial and lateral joint space width. The grade of medial/lateral PF-OA was also assessed. Inter- and intrareader agreement analyses were performed.
Findings and lessons learned
Medial PF-OA increased or appeared in 16 joints from supine to standing. The grades of lateral PF-OA were almost unchanged from the supine to the standing position.
From supine to standing position, the patellar tilt decreased, the patella moved medially, and the medial joint space width decreased. The difference in the measurements on supine and standing radiographs was assessed, and the reduction of medial joint space width, medial patellar displacement, and reduction of the patellar tilt angle were calculated.
Between 11% and 12% of the knees showed opposing direction of change in position with negative differences. The differences were significant (p < 0.0001) for all three measured parameters. Less than 15% did not change position or moved in the opposite direction. The width of lateral PF joint space was almost unchanged (p = 0.3 and p = 0.1, right and left side, respectively). Also, in joints with lateral PF-OA, the patella was displaced medially from the supine to the standing position.
For intra- and inter-reader agreement, the Altman Bland test showed a bias ≤ 0.14 for all pairs of measurements. The 95% limits of agreement were ≤ -1.6/1.8 mm for measurements of difference of joint space width and displacement and ≤ -2.2/2.10 for the difference in patellar tilt.
The authors pointed out that medial PF joint space narrowing/OA cannot be visualized by axial PF radiographs obtained in supine position, and medial PF joint space narrowing can commonly be visualized by axial PF radiographs obtained in the weight-bearing position.