After a Belgian breast screening program went digital, researchers found subtle differences in performance between digital and analog mammography systems. One of them was a major difference in radiation dose, based on whether sites used digital or computed radiography.
The Flemish Breast Cancer Screening Program was started in Flanders in 2001 using analog film-screen mammography; since 2007, sites have been transitioning to digital mammography. By the end of 2011, 78% of mammography units were using digital mammography in Flanders (European Radiology, August 2014, Vol. 24:8, pp. 1808-1819).
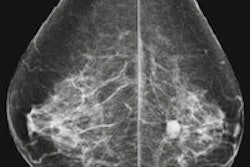
Digital mammography can be performed with either computed radiography (CR) or digital radiography (DR) technology, and which is used can affect radiation dose and performance characteristics, which are important issues affecting the program's quality, according to doctoral student Lore Timmermans, from the department of basic medical sciences at Ghent University in Belgium, and colleagues.
To test the change in radiation dose and analyze performance from the shift to digital, the researchers collected data from 975,673 mammograms from sites that digitized by either adopting CR (41 units) or DR (72 units) from 2005 to 2011. Performance indicators were obtained by consulting the screening program database.
They found that digitization produced no significant change in cancer detection rate, percentage of ductal carcinomas in situ detected, or the percentage of breast cancers detected smaller than 1 cm. However, a decrease in false-positive results and third readings (i.e., if there is discordance in interpretation between the first two readers, the mammogram is read a third time) was observed. Also, after digitization, positive predictive value (PPV) increased and recall rates decreased.
Most significantly, the researchers found that CR and DR affected radiation dose in different ways. When compared with analog mammography, mean glandular dose (MGD) for CR increases 30%, while a decrease of 30% in dose was found for DR.
Quality assurance
The stable cancer detection rate (CDR) after the transition to digital is probably testament to the program's ongoing quality assurance efforts, according to the researchers. Mammography sites are required to perform daily quality control tests for mammography systems and monitors. These tests are supervised by technical physical quality assurance organizations, which verify that systems are stable and reliable.
"This could explain the unchanged CDR as an optimally adjusted conventional device already gave its best possible CDR," they wrote. "Digital devices, which are also adjusted according to optimal settings, will generate approximately the same CDR, but the breast dose will change according to the type of digital device."
In terms of the mean glandular dose, several studies have reported dose increases when film-screen mammography is replaced by CR technology, as is the case in this study.
In terms of the detection-through-induction ratio -- considered a good indicator of mammography's risk/benefit ratio -- the cancer detection rate did not see any considerable change from film-screen mammography to DR or CR. The change in the ratio after digitization is reflected entirely by the change in breast cancer induction rate, which is dependent on the breast dose, according to the researchers.
The ratio was estimated to decrease from 48 to 36 for CR and increase from 48 to 64 for DR. The estimations are based on a relative biological effectiveness value of 4 and a dose and dose rate effectiveness factor of 2.
For the future, Timmermans and colleagues recommended that wider efforts should be made to complete follow-up data in the database. Also, in previous studies, digital mammography has proved to be better in detecting breast cancer in young women and women with dense breasts; indeed, the researchers of the current study found that for both CR and DR systems after digitization, fewer were patients classified as having dense breast tissue.
"This can be related to the better cancer detection capacity of digital mammography in dense breasts, but further investigation in this regard is necessary," they wrote.
Digital mammography will soon replace film-screen mammography entirely in the future.
"The present study has shown that quality performance parameters of the Flemish Breast Cancer Screening Program were not affected by the transition to digitalization, but a positive change over time of these parameters indicates an improvement of the entire screening program," the researchers concluded.