
Standard breast density measurement thresholds derived from film-screen mammography don't port over well to full-field digital mammography (FFDM). Using breast density assessment software, however, Canadian researchers have found that lower percentage cut points for FFDM yielded comparable prognostic power.
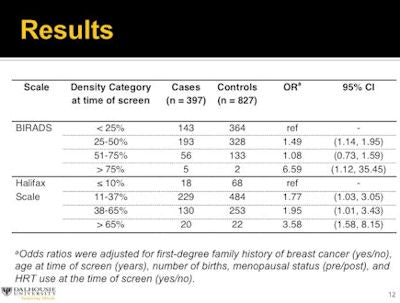
When the density measure percentage cut points were adjusted from the traditional thresholds of 25%, 50%, and 75% to 10%, 37.5%, and 65%, respectively, on FFDM, a team led by Mohamed Abdolell of Dalhousie University in Halifax, Nova Scotia, garnered breast cancer odds ratios of similar magnitude to what have been reported for film-screen mammography using quartile cut points.
"Our study is the largest case-control study that demonstrates this association between automated area-based breast density from FFDM and cancer risk," Abdolell said in an interview with AuntMinnieEurope.com.
While the current standard of care for breast density assessment is visual assessment by radiologists applying the American College of Radiology (ACR) BI-RADS density lexicon, the ACR has indicated BI-RADS assessments are not reproducible and no longer endorses its use. However, the ACR committee on BI-RADS stated, though, that they recognize physicians will continue to use density categories in mammography reports as they have done for many years, independently of BI-RADS guidance, said Abdolell, an associate professor in the department of diagnostic radiology and division of medical education/informatics.
"They go further to state that they await more robust data to support recommendation of BI-RADS density categories using validated percentage cut points that are not necessarily quartiles," he said.
Reproducible measures
Automated breast density measurement software provides reproducible measures of density but must be clinically validated, which is what Abdolell and colleagues set out to do in their study, presented at ECR 2014. Abdolell is also the founder and CEO of Densitas, which produces the software used in the study.
They wanted to determine the relationship between automated mammographic density measurements from FFDM and breast cancer risk. "Face validity" evaluated the agreement between automated mammographic density measures and radiologists' visual 2D assessments of mammographic density. "Clinical validity" evaluated the association between automated mammographic density measures and breast cancer risk.
In their case-control study of 1,287 patients, they frequency matched (1:2) a five-year age group at screening using data from the Nova Scotia Breast Screening Program and Capital District Health Authority in Nova Scotia.
Logistic regression was used to model the association between mammographic density and breast cancer risk, controlling for age, first-degree family history of breast cancer, menopausal status, number of births, and hormone replacement therapy use at time of screening. Percent density was measured from single digital mediolateral oblique views using the Densitas automated mammographic density assessment software.
The researchers used cases and controls similar in terms of number of births, hormone replacement therapy use, menopausal status, and family history. Controlling for these risk factors, women with 75% or greater density had a significantly increased risk of breast cancer compared with women who had 25% or less mammographic density.
The researchers also found the automated mammographic density measures were in "excellent agreement" with visual assessments, and, clinically, higher automated mammographic density measures were associated with increased risk of screen-detected breast cancer.
By accounting for the wider range of FFDM, the related general downshift in density values observed on FFDM, and adjusting the cut points to 10%, 37.5%, and 65%, the results show percent density measures from the Densitas algorithm validate the expected association between increased cancer risk and density, with odds ratios of similar magnitude to what have been reported for screen-film mammography using quartile cut points, Abdolell said.
The results will be verifiable by other researchers who will soon be able to access the Densitas algorithm online to validate these cut points using their own sets of digital mammograms, he added.
Future ramifications
Since ECR 2014, there have been some preliminary results showing that some mammographic density-related measures from the Densitas algorithm may be stronger predictors of breast cancer risk than any of the traditional risk factors, including age at time of screening, hormone replacement therapy use at the time of screening, menopausal status, and first-degree family history of breast cancer, Abdolell said.
The Breast Imaging EMR, built on the Caisis platform, has been identified as the synoptic reporting system for breast imaging in Nova Scotia. As a result of Abdolell and colleagues' study, a module has been developed for the Breast Imaging EMR to receive Densitas' automated density measurements so it will be possible to record density measures prospectively on every new digital mammogram.
In terms of how this study will affect breast imagers, it will add to the active discussion and understanding of the importance of rethinking cut points in FFDM and standardizing breast density measurements, Abdolell added.
"Adoption by radiologists will likely be faster and wider in scope, because they will be able to visually validate the results themselves," he said. "Further improving uptake will be the clinical validation by large case-control studies such as ours that demonstrate the strong association between automated area-based breast density from FFDM and cancer risk."
Abdolell hopes breast imagers will be in a better position with results from his study, and other similar studies, to make more evidence-based decisions about the utility and appropriateness of area-based versus volume-based density measures for clinical decision-making.
"And to appreciate that the two different approaches produce entirely different density measures that, in fact, address very different clinical issues," he said. "If masking is the key clinical issue, then area-based density measures are most appropriate. And if masking and etiology are both important clinical issues that should be considered together, then area-based measures are again most appropriate."
New initiatives
Abdolell and colleagues are continuing to pursue research activities on this topic and have broadened collaborations to include medical oncologists and pathologists.
"We have a special opportunity to do this kind of research in Nova Scotia, where opportunistic breast screening has been eliminated and all mammography is centralized, so that clinical outcomes and imaging data are available for research," he said. "There are few jurisdictions that have such population-based data with which research can be conducted."
They have also started to map out a research project with other researchers at their institution to investigate the effect of integrating automated breast density measurement in the clinical workflow. The project will focus on evaluating improved patient outcomes, reduced wait times, and improved access to care.
Study disclosures
Mohamed Abdolell is the founder and CEO of Densitas, and co-author Kaitlyn Tsuruda is an employee of Densitas.



















