
Ionizing radiation dose from medical imaging has found itself climbing the political agenda in recent years. The European Commission on Patient Radiation Safety has passed a directive prescribing measures around dose optimization that healthcare organizations in member states must implement by February 2018.
The directive is just the beginning. In my view, the Belgian government is ahead of the curve, but all members of the European Union need to be ready and able to provide in-depth data, analysis, and documentation on radiation dose metrics at any given time. A robust dose management program is the only way to deliver this.
 Dr. Jan Casselman, PhD, is the chairman of radiology at St. John's Hospital in Bruges, Belgium.
Dr. Jan Casselman, PhD, is the chairman of radiology at St. John's Hospital in Bruges, Belgium.
Having installed a hospital-wide automated dose monitoring system at St. John's, a 930-bed hospital in Bruges, I can say with conviction that this has to be the way forward for heads of radiology in hospitals around Europe. Aside from meeting the increasingly stringent criteria set by regulators, this is a matter of ethics. We need to be doing everything we can to keep dose as low as it can be, for patients and for our hospital staff.
The key to effective dose management starts with the collection, analysis, and then utilization of a hospital's dose data. The system we installed (DoseWatch, GE Healthcare) automatically retrieves, tracks, and reports on every radiation dose event administered to patients. This allows us to analyze each patient examination, review their dose history, and assess, for example, how many CT exams each patient has had, the frequency of the exams, and the patient's cumulative dose. It also allows us to compare exam study descriptions. For instance, we can compare all head CT exams from our facility, or even from a particular device, to benchmark, review, and ultimately optimize the use of dose protocols.
Day-to-day matters
I now receive an automatic email alert immediately after a scan is performed at St. John's when the scan exceeds a dose level above P95 (the five studies with the highest dose per 100 examinations for a certain protocol) or if a dose level exceeded the "threshold limit" set by our department. Of course, those exams in the top 5% may have been necessary, as some patients will require a higher dose due to their size or condition. This means we can check the reason for the outlier and understand whether it could or should be reduced in the future. If we know the dose needs to be high for a particular protocol, we can look to use scanners with the most advanced dose reduction capabilities, especially when the patient is young.
There was an instance soon after implementation, in which the data showed a particularly high dose level administered by one of our nurses. We spoke to her and discovered that she was unwittingly positioning her patients too high in the gantry, exposing them to unnecessary dose (see figure below). In time gone by, errors like this may not have been noticed, but with a dose monitoring system, all of a sudden, the invisible dose becomes visible and a hospital can take corrective action. Going forward, all hospital personnel know that when they administer an exam, it is being monitored and that adopting low-dose behavior is now a measured priority.
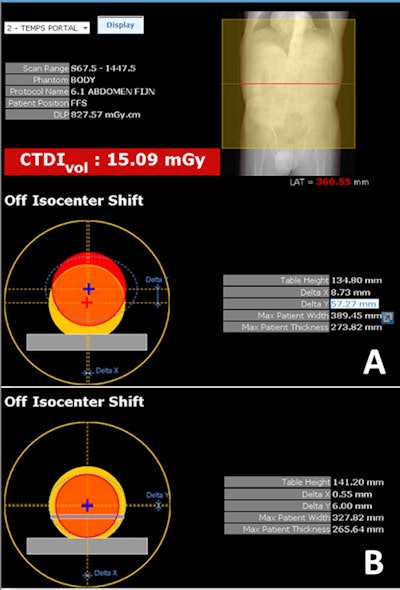 The DoseWatch software showed that the patient was positioned too high in the gantry, resulting in a higher CTDIvol (A). Correct position in the gantry (B).
The DoseWatch software showed that the patient was positioned too high in the gantry, resulting in a higher CTDIvol (A). Correct position in the gantry (B).Ultimately of course, a CT doctor will make an informed decision on whether a certain level of dose is too high for an individual exam based on the patient's clinical needs. A patient with a liver tumor, for example, who is examined on CT for the first time, will receive a higher dose than a patient who comes for a follow-up of his lymphadenopathy or liver tumor. While a dose management system may encourage doctors to consider dose thresholds, those limits can be overruled if the clinical need is justified.
Promising results
Within just a few months of implementing our system, dose levels from CT exams at St. John's fell between 25% and 30%. In the case of interventional procedures, our data monitoring encouraged us to install a new angiography room with technical capabilities to reduce dose by nearly 50%.
The combination of monitoring and a better informed department staff helped us to develop new dose protocols. Moving forward, I foresee this data being compared and contrasted between institutions, and even global regions, shining a light when dose is too high and ultimately drawing on global experience to improve patient safety in radiology departments around the world.
 After optimization, fewer outliers are seen and the majority of studies have now a CTDI less than 14, and this was 18 to 19 before (top). Before optimization, an average dose length product (DLP) of 1000 mGy·cm was used. Six months later and after optimization, DLP fell by 25% to 750 mGy·cm (bottom), as shown by the red line.
After optimization, fewer outliers are seen and the majority of studies have now a CTDI less than 14, and this was 18 to 19 before (top). Before optimization, an average dose length product (DLP) of 1000 mGy·cm was used. Six months later and after optimization, DLP fell by 25% to 750 mGy·cm (bottom), as shown by the red line.
An effective dose management system will certainly equip hospitals in EU member states to meet the new legislative requirements, but most importantly it will help radiologists to meet their ethical responsibility to ensure patient safety is as great an imperative as it can be.
Dr. Jan Casselman, PhD, is the chairman of radiology at St. John's Hospital in Bruges, Belgium.
The comments and observations expressed herein do not necessarily reflect the opinions of AuntMinnieEurope.com, nor should they be construed as an endorsement or admonishment of any particular vendor, analyst, industry consultant, or consulting group.



















