The publication by Dr. Anthony Miller and colleagues in BMJ used substandard and outdated mammography technique to claim that mammography screening would add nothing beyond what physical examination can accomplish. It takes much more than poor mammography to reach such a conclusion. Many other things would have to go wrong, and they did go wrong in the Canadian National Breast Screening trials.
A failure from the beginning
It is a well-known fact that the Canadian trials were not population-based. Instead, they used motivated volunteers who represented only 26% to 27% of the invited population. It is particularly important to note that the Canadian trials could not evaluate the independent impact of mammography because of the confounding effect of physical examination.
For these reasons, the Canadian trials were excluded from the meta-analysis of the impact of early detection using mammography on mortality from breast cancer by the World Health Organization's International Agency for Research on Cancer (IARC) workshop in 2002, even though Miller chaired the section. It is quite surprising that three authors of the current BMJ article are on record as having agreed with the following conclusions of the WHO-IARC publication (IARC Handbook of Cancer Prevention, Vol. 7: Breast Cancer Screening. Lyon: IARC; 2002):
- "There is sufficient evidence for the efficacy of screening women aged 50 to 69 years by mammography as the sole screening modality in reducing mortality from breast cancer."
- "There is inadequate evidence for the efficacy of screening women by clinical breast examination in reducing mortality from breast cancer."
- "There is inadequate evidence for the efficacy of screening women by breast self-examination in reducing mortality from breast cancer."
The scientific community, with good reason and with the assent of Miller and colleagues, excluded the Canadian trials from the assessment of mammography screening. Nevertheless, 12 years later, Miller and colleagues revert to their earlier opinion that mammography does not have an effect on mortality from breast cancer.
A total failure for many reasons
The Canadian trials stand apart as the only ones among the published screening trials that failed to show any effect on mortality from breast cancer. The flagrant professional error in figures 2 to 4 of the current BMJ paper, claiming that survival curves are actually "breast cancer specific mortality" curves, does little credit to the peer-review process carried out by BMJ as well as to the authors. The article does not provide news for anyone, since these trials have been plagued with serious quality assurance problems that have been well-known and carefully documented over the past few decades.
 Dr. László Tabár.
Dr. László Tabár.
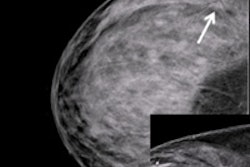
After Drs. Wende Logan and Stephen Feig resigned as outside reviewers of the Canadian trials, I (LT) was invited by Miller to review the trials' image quality. Dr. Cornelia Baines was assigned to record my evaluation of the relevant mammography quality assurance parameters for 50 selected cases from the Canadian trials.
At case 15, she terminated the review because of the overwhelmingly negative ratings given to every case. The next day at the committee meeting I should have recommended immediate termination of the Canadian trial, and I regret that I did not do so. My protests would most likely have been to no avail, as were the previous protests of Logan and Feig, followed by the vehement protests of Dr. Dan Kopans from Harvard University and Drs. Martin Yaffe and Norman Boyd from Toronto, among others.
It is worthwhile to mention the publications of Boyd and colleagues in Radiology (1993, Vol. 189:3, pp. 661-663) and in the Canadian Medical Association Journal (1997, Vol. 156:2, pp. 207-209). He and his co-authors wrote:
Questions about randomization in the [CNBSS,] however, have subsequently been raised because of the study's findings that showed an imbalance in the number of women with advanced breast cancer. In particular, the mammography arm had an excess of patients with involved axillary lymph nodes whose breast cancer had been detected by physical examination at baseline (i.e., before randomization).
Boyd's early warning about the imbalance in the number of advanced cancers in the two arms of the Canadian trials was right on target, because it is a well-known fact that the most sensitive predictor of the forthcoming mortality results in a screening trial is whether or not the screening in question decreases the advanced cancer rate. The Canadian trials are the only ones among all the trials that did not report any decrease in the advanced cancer rate. This is not surprising because of the above mentioned imbalances, but also because the radiologists were not trained for the demanding task of finding early breast cancers.
Boyd and co-authors also wrote:
We now know that names were altered and that there were more alterations in the mammography arm. Although 78% of these changes could be accounted for in some way (e.g., clerical errors), the remaining 22% (representing 101 names) could not. We also now know that a coordinator at one of the [CNBSS] centers was suspected of assigning her friends to the mammography arm and that the suspicion was strong enough to remove her from her position. We do not know the method of subversion thought to have been used by this coordinator, nor do we know whether an examination of name alterations revealed what she was alleged to have done.
Comparison with other trials
There is no comparison, since the Canadian trials are uniquely poorly designed and carried out and, therefore, have been much criticized for decades. Miller and his colleagues make an attempt to compare the Canadian trials only with the Swedish Two-County Trial, although their subtitle is "Comparison with other studies."
Comparing the Canadian trials with the Swedish Two-County Trial is inappropriate for many reasons, and the statements published in the BMJ article are contrary to fact:
- The randomization did not take place on a "county level" as the authors claim, since a Swedish county corresponds to a province in Canada or a state in the U.S.
- The average tumor size in the control group was not 28 mm but 22 mm.
- Their false claim that the significant reduction in mortality observed in women invited to screening in the Swedish trial is due to an initial imbalance has already been shown to be unfounded, and Miller and his colleagues should be aware of this publication (Duffy et al, Annals of Oncology, 2003, Vol. 14:8, pp. 1196-1198).
- The fact that mortality from breast cancer was compared among women invited versus those not invited implies that the true impact of screening among those who actually attended was considerably higher than 31%.
- The Swedish Two-County Trial was population-based while the Canadian trials were not.
The following data can inform the reader about the true difference between the CNBSS and the Swedish Two-County Trial: The Swedish trial did decrease the advanced cancer rate in women invited to screening, whereas the Canadian studies had an excess of advanced cancers in the mammography arm.
According to the original report of CNBSS, the relative rate of node-positive cases in the mammography arm versus the control arm in the 40 to 49 age group and the 50 to 59 age group were 1.53 (95% confidence interval [CI]: 1.11-2.09) and 1.07 (95% CI: 0.80-1.44), respectively, and 1.27 (95% CI: 1.02-1.57) for the two age groups combined. The failure to reduce advanced breast cancer therefore resulted in the lack of benefit in reducing breast cancer mortality in CNBSS.
In contrast, the corresponding figure of reducing advanced cancer for women ages 40 to 74 was 0.75 (95% CI: 0.65-0.87) as reported in the first article of the Swedish Two-County Trial (Tabár et al, 1985). The reduction in advanced breast cancer also led to a 31% reduction in mortality from breast cancer in women invited to screening.
Miller and colleagues' current article in BMJ confirms Boyd's conclusion published 21 years ago in Radiology (1993, Vol. 189:3, pp. 661-663):
Taken at face value, the results of the [CNBSS] argue for abandoning mammographic screening as a population-based means of controlling death rates from breast cancer. We believe such a conclusion to be unjustified and unsupported by the findings of the [CNBSS] ... [and] the results of these trials should not be used to change the prevailing scientific view of the potential benefits of screening with mammography.
Dr. László Tabár is professor emeritus of radiology at University of Uppsala School of Medicine and former medical director of the department of mammography at Falun Central Hospital.
The comments and observations expressed herein do not necessarily reflect the opinions of AuntMinnie.com and AuntMinnieEurope.com.