Researchers from Geneva collected a prestigious Magna Cum Laude award at the recent RSNA 2013 meeting in Chicago for their studies on diffusion-weighted imaging (DWI) and PET/MRI. They were one of only five European groups who received the top prize for their education exhibits.
"Interpretation of MRI findings after radiation therapy of head and neck cancers constitutes a diagnostic challenge," noted Dr. Arthur Varoquaux, from the department of radiology at Geneva University Hospital, and colleagues. "DWI-MRI and PET/MRI increase the diagnostic confidence for the detection of recurrent tumors and help to avoid unnecessary biopsy."
More learning tools must be made available for imaging of the irradiated head and neck, they stressed. Interpreting imaging studies of the irradiated neck is challenging due to radiotherapy-induced tissue alterations, variable appearance of recurrent tumors, and functional phenomena mimicking disease. MRI, DWI, PET/CT, and software fusion of PET and MRI data are increasingly used in clinical routine, and because MRI and PET often yield complementary information, hybrid PET/MRI systems hold promise to facilitate differentiation of tumor recurrence from post-therapeutic changes and complications, according to Varoquaux et al.
"Hybrid PET/MRI systems enable acquisition of anatomic, functional, and metabolic information in the same session. Three types of hybrid systems exist: PET/MRI (PET and MRI integrated in the same gantry), sequential PET/MRI (two separate scanners in the same room using a common rotating table), and sequential PET/CT-MRI (separate PET/CT and MRI scanner in two adjacent rooms with a transferable patient table that can be docked on either scanner)," they explained.
The authors' study population included 124 consecutive patients imaged over four months -- 22 years after radiotherapy ± chemotherapy for head and neck squamous cell carcinoma, lymphoma, and other malignant head and neck tumors. DWI-MRI was available in all 124 patients. In 28 patients, head and neck MRI and whole-body PET/CT exams were performed on two separate scanners, and in 31 patients whole-body PET/MRI was obtained on a sequential hybrid PET/MRI system. The PET tracer used was F-18 FDG, and imaging findings were correlated with histology in 82 patients and radiologic follow-up over more than 12 months in 42 patients.
The fusion of functional, metabolic, and corresponding anatomical MR images was done using a commercially available software algorithm or was achieved by hardware fusion. Apparent diffusion coefficient (ADC) values and standardized uptake values (SUV) were determined in all patients.
DWI is a functional MRI technique that assesses the random (Brownian) motion of water molecules, the authors reported. In the presence of biologic barriers, the free displacement (diffusion) of water molecules is restricted. In clinical routine, the ADC mean is often used for quantification, and quantification of tracer uptake on PET is done by calculating SUVmean and SUVmax using CT or MRI-based attenuation correction methods.
The researchers identified the following pitfalls:
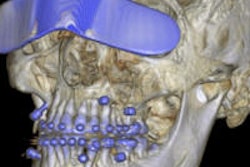
Susceptibility artifacts due to dental hardware. These artifacts are more pronounced at high field strength and on DWI sequences. They lead to spatial distortion of the surrounding anatomy, especially on DWI, resulting in underestimation of tumor size and of invasion into adjacent structures. Susceptibility artifacts also affect SUV measurements on PET/MRI.
Miscoregistration artifacts. These are caused by geometric distortion and patient motion. Fusion of geometrically distorted DWI sequences with morphologic MRI sequences can lead to erroneous interpretation of tumor localization. Motion and respiratory mismatch between MRI and PET data can also result in anatomic miscoregistration, which can cause diagnostic errors with respect to precise tumor localization or extension. Careful analysis of all datasets is essential.
Inadequate scanner resolution and low FDG avidity. FDG-PET may miss small tumors because these lesions are below the resolution of current PET scanners. Therefore, false-negative results can occur, especially regarding metastatic lymph nodes in the neck. Some malignant tumors (well-differentiated sarcomas and necrotic tumors) are not FDG-avid, so PET may yield false-negative results. The complementary information obtained by DWI-MRI decreases the number of false-negative interpretations.
False positives due to inflammatory findings. Inflammatory or infectious conditions, as well as benign pathologies, can lead to false-positive PET assessments, and correlation with DWI findings often helps to solve the diagnostic dilemma. A common problem in clinical routine is the coexistence of inflammatory findings and tumor recurrence, making precise preoperative assessment of tumor margins challenging. Iatrogenic focal uptake from recent surgery, tracheostomy cannula replacement, gastric tube, biopsy, endosseous implants, or dental extractions are frequent, and image interpretation is usually straightforward.
Incidentalomas. These incidental findings are present outside the targeted organ. Thyroid incidentalomas represent benign nodules, but malignant lesions (mainly papillary thyroid cancers) can be seen in 20% of incidentally discovered thyroid lesions. Further head and neck incidentalomas detected on PET/MRI include Warthin's tumors (3% in the authors' series) and lymph nodes with high tracer uptake due to granulomatous diseases (3% in their series). Other incidentalomas (7% in their series) comprise cholesteatomas, intracranial and abdominal aneurysms, dentigerous cysts, vestibular schwannomas, clivus hemangiomas, dermoid cysts, lipomas, and parathyroid adenomas. Detection of intecidentalomas requires further diagnostic workup.