Change in F-18 fluorothymidine (FLT) uptake on PET during early radiotherapy or chemoradiotherapy is a strong indicator of the long-term outcomes of head and neck cancer patients, according to a study published in the April issue of the Journal of Nuclear Medicine.
Dutch researchers found that better three-year disease-free survival was associated with a maximum standardized uptake value (SUVmax) decrease of at least 45%, as well as a gross tumor volume decrease matching at least the median, during the first two weeks of treatment.
FLT-PET scans conducted in the second week of treatment were most useful in personalizing patient treatment, wrote Dr. Bianca Hoeben, from the department of radiation oncology at Radboud University Nijmegen Medical Centre, and colleagues (JNM, April 2013, Vol. 54:4, pp. 532-540).
Early intervention
The ability to visualize the progression of tumor cells can lead to early changes in treatment and potentially improve patient outcomes, according to the authors. Based on newly discovered tumor characteristics and the individual patient's case, more aggressive therapy such as chemotherapy, accelerated radiotherapy, or a combination of treatments may be warranted.
"In individualized therapy strategies, additional information from FLT-PET could be of complementary value in intensifying treatment if needed and, possibly, in de-escalating treatment when early evaluation indicates high responsiveness," Hoeben and colleagues wrote.
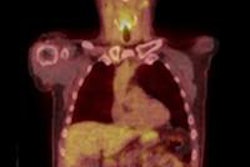
In the study, 48 patients with squamous cell carcinomas of the head and neck underwent consecutive FLT-PET/CT scans between July 2006 and August 2008. The goal was to determine if early changes in tumor uptake volume and signal on FLT-PET could predict long-term clinical outcome, they wrote.
Participants were at least 18 years old, had newly diagnosed stage II to stage IV squamous cell carcinoma, and received radiotherapy with or without concomitant chemotherapy. Subjects were excluded if they had surgery as their primary tumor therapy, had palliative treatment, and/or were pregnant.
Integrated FLT-PET and CT images were acquired on a hybrid PET/CT scanner (Biograph Duo, Siemens Healthcare) 60 minutes after intravenous injection of 250 MBq of FLT. Scans were conducted in two bed positions over the head and neck area at seven minutes per bed position in 3D mode.
Patient therapy
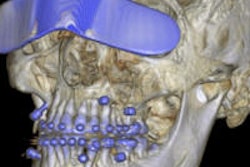
Of the 48 patients, 18 received 3D conformal radiotherapy, while the other 30 were given intensity-modulated radiation therapy (IMRT) for primary tumors, metastatic cervical lymph nodes, and electively treated nodes. Follow-up was every two months in the first year, every three months in the second year, every four months in the third year, and every six months in the fourth and fifth years.
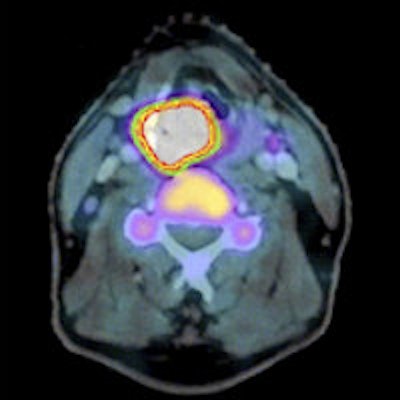
All patients underwent FLT-PET/CT before radiotherapy (median, four days; range, 0 to 14 days), and all but two patients received FLT-PET/CT in the second week after a median of seven radiotherapy fractions (range, five to 12 fractions).
After amending the study protocol, 29 patients also underwent a third scan in the fourth week of treatment after a median of 18 fractions (range, 15 to 19 fractions).
"The reason for this third scan was to investigate whether the substantial decrease in FLT uptake after one week continued or whether tumor cell repopulation occurring later during the course of treatment might increase FLT uptake again," the authors explained. "After completion of therapy, all patients showed a complete local response."
In their analysis, Hoeben and colleagues found that when SUVmax decreased at least 45% and gross tumor volume using visual delineation (GTVvis) decreased at least 31% (the median) during the first two weeks of treatment, three-year disease-free survival was 88%, compared with 63% for other patients.
A GTVvis decline greater than the 31% median in the fourth treatment week was also associated with better three-year locoregional control, at 100% compared with 68% for other participants.
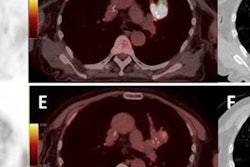
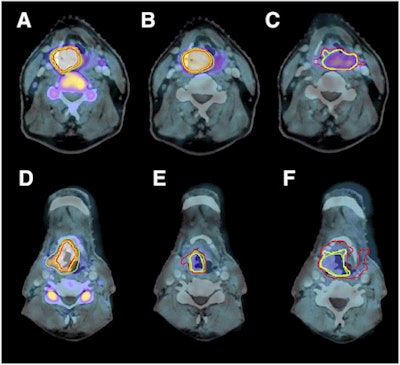 FLT-PET/CT images of laryngeal carcinoma before therapy (A and D), in second week of therapy (B and E), and in fourth week of therapy (C and F). Images A, B, and C show a slow decrease in FLT uptake, while D, E, and F show a fast decrease in FLT uptake. Image courtesy of JNM.
FLT-PET/CT images of laryngeal carcinoma before therapy (A and D), in second week of therapy (B and E), and in fourth week of therapy (C and F). Images A, B, and C show a slow decrease in FLT uptake, while D, E, and F show a fast decrease in FLT uptake. Image courtesy of JNM.The association was most pronounced in the patients who received chemoradiotherapy: Within this group, disease-free survival was 100% for those with at least a 31% decrease in GTVvis after two weeks of treatment, compared with 50% for those with a less than 31% decrease. Among patients who received only radiotherapy, there was no statistically significant difference until the fourth week of treatment.
The best time to perform FLT-PET scans is during the second week of treatment, the authors also noted.
"Later measurements did not add much information, and the FLT-PET signal became more difficult to quantify because of decreasing signal-to-noise ratios," they wrote. "In addition, if adjustments of the treatment strategy are anticipated, these should be decided as early as possible after the start of therapy."
"Given the notion that tumor cell proliferation is a mechanism of therapy resistance, FLT-PET should provide an effective tool for decisions on early and personalized treatment adaptation in patients with head and neck cancer," the authors concluded.