Digital breast tomosynthesis (DBT) has been praised as a powerful tool in the breast imaging armamentarium, but these 3D studies can also be time-consuming and complicated for radiologists to interpret. Computer-aided detection (CAD) technology may be of assistance, Italian researchers have found.
In a retrospective review, CAD software yielded 89% sensitivity for malignant lesions, including 86% for masses and 95% for microcalcification clusters.
"Our preliminary results are comparable to those observed for conventional CAD systems on [2D digital mammography images] reported in the literature," said Dr. Manuela Durando of A.O.U. San Giovanni Battista in Torino. She presented the findings during a scientific session at the RSNA 2013 meeting in Chicago.
An important role?
While DBT offers increased sensitivity for detecting breast cancer, better lesion characterization, and a decrease in recall rates over conventional mammography, DBT studies can have more images and information to review, which may increase radiologist reading times. As a result, the role of CAD could be important in DBT in order to maintain current clinical workflow with large 3D datasets, Durando said.
Because the performance of CAD for DBT hasn't been well-established, the research team sought to evaluate the performance of the CAD Breast DTS system (im3D) for detecting lesions at DBT on an independent testing set. The research team included several employees of im3D, an Italian CAD software developer.
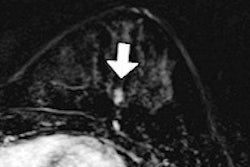
They retrospectively evaluated the software, which is designed to identify both masses and microcalcification clusters, on a test set of 143 cases. The 143 patients received craniocaudal (CC) and mediolateral-oblique (MLO) DBT projections on a Selenia Dimensions full-field digital mammography system (Hologic), generating 484 breast volumes. The DBT projections were reconstructed using the Briona tomosynthesis 3D image reconstruction software library (Real Time Tomography) prior to receiving CAD.
The 143 cases included 84 biopsy-proven malignant lesions with a mean size of 23 mm (standard deviation = 18 mm). These 84 malignant lesions included 59 masses or architectural disorders, 19 microcalcification clusters, and six masses with associated microcalcifications. There were 64 benign lesions (proved with biopsy or follow-up) with a mean size of 18 mm (standard deviation = 14 mm).
The CAD software was trained on a separate set of DBT cases that weren't included in the study, and then applied to the breast volumes.
After an experienced radiologist drew a 3D bounding box around each malignant lesion view, the annotations were then compared with the CAD marks. The researchers considered a lesion to be detected if it was identified by CAD on either the CC or MLO view.
A true CAD positive was registered for masses when the CAD marking overlapped the radiologist marking by at least 20%, she said. For microcalcifications, the team tallied a CAD true positive when at least two of the microcalcifications identified by the radiologist fell within the CAD marking. Masses with associated microcalcifications were considered correctly identified if the software marked at least a mass or a microcalcification cluster, according to the group.
The researchers then calculated sensitivity and false positives per breast volume, as well as the distribution of BI-RADS breast density categories.
High sensitivity
Overall, CAD detected 75 of 84 malignant lesions for a sensitivity of 89% (Confidence interval: 95%: 81-94%).
Sensitivity of CAD software by lesion type:
- Masses only: 51/59 lesions: 86%
- Microcalcification clusters: 18/19 lesions: 95%
- Masses + microcalcification cluster: 6/6 lesions (100%)
There were an average of two false positives/per view presented as masses and one false-positive per view presented as a microcalcification, Durando reported.
| CAD results by patient BI-RADS breast density classification | ||||
| Number of patients | Malignant lesions | Sensitivity | Mean false positives per view | |
| BI-RADS 1 and 2 | 62 | 35 | 34/35 (97%) | 3 ± 2 |
| BI-RADS 3 and 4 | 81 | 49 | 41/49 (84%) | 3 ± 2 |
"The sensitivity was higher in nondense breasts than in dense breasts, but there were no differences in false positives," she said.
The CAD software's sensitivity and false-positive rate was comparable with those reported in the literature for other commercial CAD systems used with standard digital mammography studies.
Durando noted that the software's sensitivity and, in particular its specificity, should be further improved in order to be clinically useful. She also acknowledged limitations of the study, including the need to validate the findings on a larger cohort of patients, including negative cases with follow-up and/or cases from a screening population, she said. In addition, the researchers only studied the standalone performance of the CAD system and did not explore CAD/radiologist interaction.