
Use of automated breast ultrasound (ABUS) in combination with mammography for women with dense breast tissue can result in an increase in cancer detection from 0.42% with mammography alone compared with 0.66% in women who received mammography combined with ABUS, according to a new European study.
The European Asymptomatic Screening Study (EASY) investigated the effectiveness of the somo-v ABUS system by assessing cancer recall, biopsy, and detection rates for the combination of full-field digital mammography (FFDM) and ABUS, compared with mammography alone. It was led by Dr. Karin Leifland, PhD, head of the Unilabs mammography department at Capio St Göran's Hospital in Stockholm.
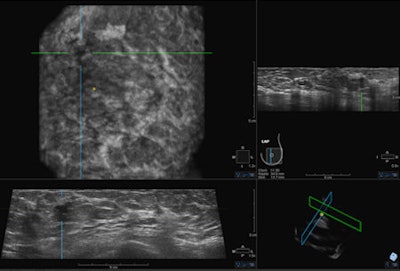 Last September the U.S. Food and Drug Administration (FDA) approved the somo-v ABUS device for use in combination with mammography in women with dense breast tissue. This may drive increased interest from physicians in the use of ultrasound as a screening tool. Image courtesy of GE Healthcare.
Last September the U.S. Food and Drug Administration (FDA) approved the somo-v ABUS device for use in combination with mammography in women with dense breast tissue. This may drive increased interest from physicians in the use of ultrasound as a screening tool. Image courtesy of GE Healthcare."This study actually demonstrates a 57% rise in finding breast cancer compared to the overall statistics for the year before," she told AuntMinnieEurope.com. "Together with studies in the United States, this study shows that adding ABUS to mammography finds 50% more cancers in the screening program, and more importantly, the cancers would be found when smaller and at an earlier stage."
Mammography can be of relatively limited value for women with dense breast tissue, as identified by women who have more glandular tissue (greater than 50%) than fatty tissue. "In fatty tissue the sensitivity of mammography can be high, 80% to 90%, but in dense breast tissue the sensitivity drops to about 62%," said Dr. Jessie Jacob, radiologist and vice president of medical affairs at U-Systems, part of GE Healthcare, which developed the somo-v ABUS system.
In addition, having dense breast tissue carries a four to six times increase in risk compared with women with fatty tissue. More than half of women younger than 50, and about 30% of women older than 50, have dense breasts.
"Dense tissue affects a large number of women and the difficulty is in finding a technique that can be applied to so many women effectively, to supplement mammography," Jacob added.
 In dense breast tissue, the sensitivity of mammography drops quite dramatically, according to Dr. Jessie Jacob.
In dense breast tissue, the sensitivity of mammography drops quite dramatically, according to Dr. Jessie Jacob.
Evidence suggests that using handheld ultrasound in conjunction with mammography can increase the sensitivity of mammography by up to 90%, but there are considerable problems related to handheld ultrasound, e.g., operator inconsistency with variation in identification of benign or malignant tissue.
The somo-v ABUS system was specifically designed not only for screening dense breast tissue, but also to operate efficiently in the screening environment. Being automated in nature, the device is operator independent and is associated with enhanced consistency, and the radiologist only needs to interpret the images rather than necessarily conducting the scan, aiding workflow, and managing time efficiency, she explained.
The results of the EASY trial were presented at the recent European Cancer Congress (ECC) by Alexandra Schulz, clinical marketing manager for ultrasound at GE Healthcare. A total of 1,676 asymptomatic women between 40 and 74 years of age with dense breast tissue participated in the screening study.
All women received a mammogram and an ABUS screen. The first radiologist read the mammogram, blinded to the ABUS, and then read the ABUS later. A second radiologist also read the mammogram study to confirm the findings, so effectively there was a double reading.
If the first reader decided the mammogram and the ABUS were both normal, the second reader only looked at the mammograms. But if the first reader questioned either the mammogram or the ABUS, the second reader read the ABUS scan in addition to the mammogram.
The researchers found that supplementing mammography with ABUS significantly increased the cancer detection rate from 4.2 in 1,000 to 6.6 in 1,000. "The success of a breast screening program is in finding breast cancer when it is as small as possible, and with the combination of mammography and ABUS in dense breast tissue, tumors can be found at an earlier stage," Leifland remarked. "Hopefully this will lead to further lowering of mortality in the screening population."
A total of 38 women (2.3%) who underwent mammography combined with ABUS were recalled compared with 3% who were recalled for mammography alone in 2010 (the study ran from 2010 to 2012). The lower number of recalls when ABUS was used to supplement mammography was even more surprising given these women had dense breast tissue, in which it is harder to find cancers with mammography alone.
Leifland explained that ABUS probably showed areas that were hard to determine by mammography alone because of the tissue density, but an ABUS scan would clear some of these areas.
Of the 38 recalls, 14 were due to mammography findings where the associated ABUS reading was normal or abnormal. Nine of these 14 women subsequently had needle biopsies, with seven confirmed malignancies. Of particular note, 24 out of 38 women were recalled for ABUS findings after a normal mammography reading. Four of these 24 women had cancer that was not seen on mammogram but only on ABUS.
Finally, all the cancers identified by the combination of mammography and ABUS were invasive cancers. This is significant because around 20% of cancers identified by mammography alone are ductal carcinoma in situ, of which only 20% to 30% progress to the invasive form. With ABUS, every cancer found was an invasive, node-negative cancer.
Asked about the significance of using the ABUS scan in screening procedures, Leifland said she considered the current screening program to be very good, especially in women with less than 50% dense tissue, lowering breast cancer mortality by more than 30%. "But more needs to be done for women with dense breast tissue. Studies in high-risk women have shown a sensitivity for mammography of less than 50%."
In Europe, the somo-v ABUS system has not yet received its CE Mark.



















