FDG-PET/MRI more accurately evaluated and more often changed the management of patients with various forms of cancer in a comparison with PET/CT, according to preliminary research conducted in Naples, Italy, and the U.S.
Researchers found that PET/MRI outperformed PET/CT for swollen lymph nodes (lymphadenopathy) and tumors in regions that were difficult to assess with PET/CT, such as the kidneys, and achieved greater sensitivity with bony and hepatic metastases.
Among 134 patients in the study, PET/MRI provided additional information that affected clinical management for 24 (18%), wrote lead author Dr. Onofrio Catalano, from the department of radiology at SDN Istituto Ricerca Diagnostica Nucleare in Naples, Italy, and colleagues (Radiology, 5 September 2013).
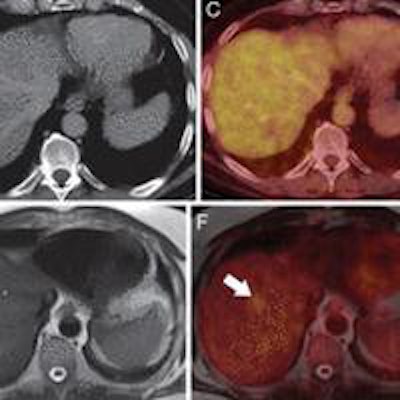
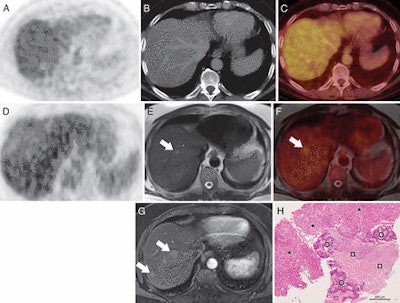 Images are of a 66-year-old man at follow-up for colorectal cancer. PET (A), CT (B), and PET/CT (C) images show no lesions. However, PET (D), T2-weighted MRI (E), and fused PET/MRI (F) show two liver metastases (arrow) that were confirmed on contrast-enhanced ultrasound and biopsy. The patient underwent radiofrequency ablation with ultrasound guidance. Images courtesy of Radiology.
Images are of a 66-year-old man at follow-up for colorectal cancer. PET (A), CT (B), and PET/CT (C) images show no lesions. However, PET (D), T2-weighted MRI (E), and fused PET/MRI (F) show two liver metastases (arrow) that were confirmed on contrast-enhanced ultrasound and biopsy. The patient underwent radiofrequency ablation with ultrasound guidance. Images courtesy of Radiology.PET/MRI vs. PET/CT
Over the past decade, FDG-PET/CT has often been the modality of choice for oncologic imaging, the authors noted. However, the newer hybrid modality PET/MRI has shown promise for the same clinical applications.
MRI has better soft-tissue contrast-to-noise ratio, for example, in the abdomen, pelvis, and central nervous system compared to CT, and without the radiation. In addition, physicians can evaluate tissue function with diffusion-weighted MRI, MR spectroscopy, and perfusion-weighted imaging.
"These MR features, combined with the metabolic information from PET, suggest the potential for PET/MRI to have an extensive effect on patient care," the authors wrote.
The retrospective study by Catalano and colleagues surveyed consecutive patients scheduled for same-day FDG-PET/CT and FDG-PET/MRI between February and September 2012 for oncologic staging or follow-up for neoplasms outside the central nervous system.
Subjects were excluded if they were pregnant; had inadequate PET/CT images, PET/MR images, or both due to artifacts, system malfunction, or poor patient cooperation; had a contraindication to MRI; or could not handle being in the PET/MRI scanner. The final patient cohort included 82 women and 52 men, with a mean age of 57.9 years (± 13.6 years).
Imaging protocols
PET/CT exams were conducted on a 64-detector-row system (Gemini TF, Philips Healthcare) approximately 60 minutes (± 7 minutes) after FDG injection (mean dose, 4.44 MBq/kg). Scans were conducted from the midthigh to the cranium, either with or without contrast.
PET/MRI studies were acquired using a 16-channel head and neck surface coil and three or four 12-channel body coils, depending on the patient's height (Biograph mMR, Siemens Healthcare). PET/MRI protocols were chosen based only on the clinical indications, without knowledge of PET/CT findings. If contrast was requested, clinicians used 0.1 mmol/kg of gadopentetate dimeglumine (Magnevist, Bayer HealthCare Pharmaceuticals). PET/MRI scans began approximately 88 minutes (± 29 minutes) after FDG injection and lasted for a mean of 66 minutes (± 12 minutes).
The analysis showed that PET/CT and PET/MRI findings agreed for 73 (54%) of the 134 patients, according to Catalano and colleagues.
PET/MRI discovered additional abnormalities not seen at PET/CT in 55 patients (41%) and altered treatment for 24 (18%). PET/MRI findings that affected clinical management included metastases in six patients, which led to chemotherapy, and incidental neoplasms followed by surgery in four individuals. It also ruled out malignancy in six patients.
PET/CT revealed additional findings not seen on PET/MRI in six (4%) of the 134 patients, detecting lung nodules smaller than 6 mm. The findings did not influence clinical management for four patients (3%), but they did lead to chest CT follow-up for two patients (1.5%).
Catalano and colleagues concluded that PET/MRI was more accurate than PET/CT for evaluating lymphadenopathy, and it was more sensitive to bony and hepatic metastases than PET/CT. "PET/MR imaging proved capable in the evaluation of tumors in regions that were difficult to assess with PET/CT, such as the kidneys," they added.
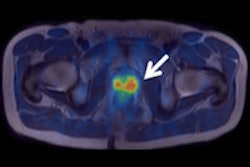
"In our cohort of patients, primary and secondary lesions in the kidneys were challenging to identify on PET/CT images, and their FDG uptake was often misinterpreted as urinary activity; however, correlation with MR images enabled us to detect unsuspected renal cancers in three patients and renal metastases in one patient," the group wrote.
Treatment changes
The most common treatment changes based on PET/MRI results were the initiation of chemotherapy for seven patients (5.2%), avoidance of biopsy in six (4.5%), and adding surgery for five (3.7%).
The authors cited several study limitations, including the potential for selection bias due to the retrospective approach to the research. They also noted that PET/MRI is still relatively new and "experience and consensus regarding imaging protocols is lacking."
"However, even for PET/CT, there is still no consensus regarding a standard set of scanning protocols," they wrote.
Study disclosures
Two study authors are consultants for Siemens.