Pooled blood volume (PBV) images from dual-energy CT (DECT) can be a powerful tool to differentiate clinically important pulmonary embolism (PE) from less important filling defects, and can even help clinicians manage pulmonary hypertension (PH), concluded a talk at the 2013 International Symposium on Multidetector-Row CT.
Earlier studies showed results on PBV images of the chest correspond to other measures of the severity of such difficult-to-assess conditions as pulmonary embolism and chronic thromboembolic pulmonary hypertension. It's time to refine the use of PBV images to improve the management of these patients, said Dr. Johnny Vlahos from St. George's Hospital in London.
"Pulmonary hypertension is a life-threatening condition with an insidious onset, and often the diagnosis is made in a very delayed fashion," Vlahos said. Evaluation with CT is key to identifying the presence or the severity of PH, as well as the underlying cause or multifactorial causes of it."
New research is creating a functional element to pulmonary hypertension assessment that could lead to better patient outcomes, but CT alone has a problem providing the necessary perfusion and functional information required to make a diagnosis.
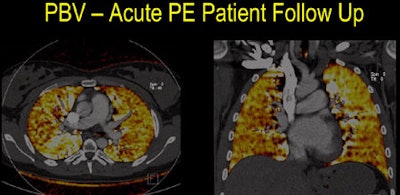 Above, patient with a large filling defect in lower left lobe had evolved at follow-up six months later, and the patient had a very good outcome. Conversely, patient below with extensive thrombus and extensive PBV defects worsened over six months, retaining extensive pulmonary emboli and defects, and developing thromboembolic pulmonary hypertension. All images courtesy of Dr. Johnny Vlahos.
Above, patient with a large filling defect in lower left lobe had evolved at follow-up six months later, and the patient had a very good outcome. Conversely, patient below with extensive thrombus and extensive PBV defects worsened over six months, retaining extensive pulmonary emboli and defects, and developing thromboembolic pulmonary hypertension. All images courtesy of Dr. Johnny Vlahos.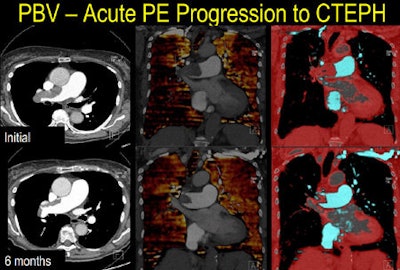
"CT without dual energy is very helpful in perhaps suggesting the diagnosis or determining the underlying etiology, but CT is deficient in its conventional form when trying to decide what type of therapy these patients may use, especially some of the newer therapies that may be detrimental in some patients," Vlahos said. Other functional imaging exams must be recruited to fill the gap, including echocardiography or sometimes ventilation/perfusion (V/Q) imaging.
Certainly the evidence to date suggests an important role for DECT and pulmonary blood volume imaging in PH and PE, he noted. To begin, the most physiologically impairing occlusive PE are associated with perfusion defects on PBV imaging, while nonimpairing PH cases do not cause perfusion defects at PBV imaging, providing a handy way to identify more serious cases. Several studies have shown that PBV defects are more common in patients who have occlusive filling defects versus nonocclusive defects.
For example, in 2006 Pontana et al looked at 177 patients using blood pool imaging on DECT. The images showed PBV defects in 14 of 17 occlusive pulmonary emboli, while showing defects in just five of 58 nonocclusive emboli. In 2009, Thieme and colleagues examined 93 patients with suspected PE. PBV images showed defects in 42 of 44 occlusive pulmonary emboli but just two out of 33 nonocclusive PE.
Third, the more PBV defects the more likely the patient is to have severe right ventricular impairment and a poor prognosis, he said. "So it's reasonable to suggest that the extent, severity, and right heart strain are worse when you have more PBV defects, and at least for thromboembolic hypertension this probably also applies," he said. "Perhaps PBV imaging is an index of the prognosis in patients with chronic thromboembolic hypertension."
Finally, when patients with established small triangular defects but no PE are treated for PE, these defects tend to resolve as well, suggesting that the triangles may represent the kind of small peripheral microemboli that are seen on V/Q scans.
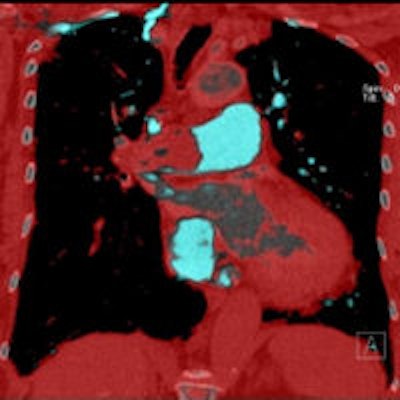
"When we image patients with CTEPH [chronic thromboembolic pulmonary hypertension] with PBV, we see far more severe defects than we would see in patients with acute pulmonary embolic disease," Vlahos said. Also, the presence of subtle mosaic attenuation patterns at CT tends to correlate with PBV defects, especially in areas of low attenuation.
In several studies that have looked at variations in patients undergoing PBV imaging, the defects at PBV have tended to occur where the CTEPH deficits were most severe, particularly where there are strictures and bands in the pulmonary arteries. Thus, PBV provides important functional and physiological information on PE severity, and may also have a role in predicting prognosis and progression to chronic thromboembolic disease, he said. The same subtle mosaic attenuation is seen not only in CTEPH cases but in other conditions with pulmonary hypertension as well, he added.
In Vlahos' facility, patients presenting with acute PE and large filling defects are now followed to see how they progress, he said.
PE, PH, and new research efforts
In a new study slated for presentation at the RSNA 2013 meeting by Rahani and colleagues, Hounsfield unit (HU) enhancement at PBV is also correlated significantly to the presence of PE, Vlahos said. The retrospective review of nearly 100 patients shows that mean enhancement in the central in the pulmonary artery was lower (HU = 252) in patients without PE compared with patients with PE (HU = 277, p = 0.005), he said.
"If you look at the group that has pulmonary hypertension, they generally have higher levels of contrast opacification in the central pulmonary arteries compared with non-PH patients," he said. Conversely, patients without PH had higher enhancement of the lung parenchyma compared with PH patients. "That suggests that in patients with PH there's a delay in getting the contrast from the central arteries out into the lung parenchyma," Vlahos said.
Similarly, a study looking at attenuation variance in six automatically generated regions at PBV correlated with pulmonary vascular resistance, as expressed in 3D lung regional enhancement variance versus pulmonary vascular resistance (PVR): (r = 0.44, p < 0.05).
New data to be presented this year also show that heterogeneity of the lungs analyzing standardized lung volumes with PBV images correlates moderately well with pulmonary vascular resistance (PVR), which is the key determinant for treating patients with pulmonary hypertension, and could therefore potentially guide management, Vlahos said. This study calculates the pulmonary artery to whole lung enhancement ratio, and found that it correlated to PVR (r = 0.59, p < 0.01).
Finally, a new prospective study is underway to determine what information can be gleaned from dual-time point imaging with PBV, with images acquired during an initial peak phase followed by a limited slab acquisition through the central pulmonary arteries. For the most part, patients are showing the same enhancement patterns in the delayed phase as in the initial phase, Vlahos said. But remember that patients with PH have reduced parenchymal enhancement that nevertheless endures for a longer time than normal patients, so a PH patient might have large deficits in the parenchymal phase that fill in by the aortic phase.
"I'd like to postulate that pulmonary blood volume imaging and pulmonary thromboembolic disease is a very useful technique, and probably can be very useful if it's standardized," Vlahos said. "Variability in this PBV measurement may reflect pulmonary vascular resistance, and may in the future guide therapy or monitor therapy, and therefore may bring a functional element to the evaluation of pulmonary hypertension that was previously lacking."