The U.K. Royal College of Radiologists (RCR) has updated its guidelines on the measures routinely taken in imaging departments to protect unborn children from irradiation.
The current practice is to ask women of childbearing potential if there is any chance they might be pregnant. If the answer is anything other than a definite "no," the radiographer or radiologist must check the date of the last menstrual period, explained Dr. Pete Cavanagh, RCR's vice president, clinical radiology, who wrote the new document, "Radiation and the Early Fetus" (Ref No: BFCR[13]4).
"When the period is overdue and the patient cannot be certain she is not pregnant, consideration will be given to postponing the examination. This will usually require consultation with the responsible radiologist, and they may need to have a discussion with the referring clinician. This is the '28-day rule,'" he explained. "The 28-day rule replaced the 10-day rule introduced in 1986, but there is evidence the incidence of childhood cancer may be increased slightly following in utero irradiation before a period has been missed."
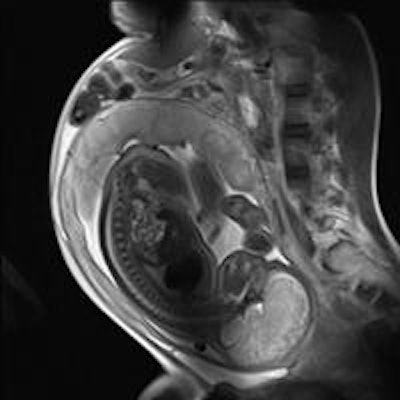
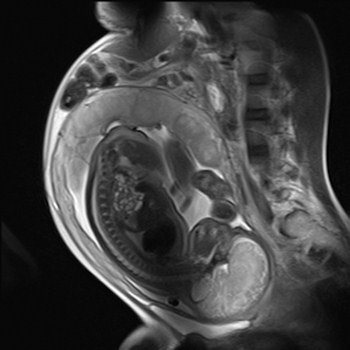 Imaging can provide exquisite details of the fetus. This sagittal half-Fourier acquisition single-shot turbo spin-echo (HASTE) MR image was used for planning further fetal images in other planes, and was taken at the Clinical Research Imaging Center, University of Edinburgh, U.K. Image courtesy of Janet De Wilde, PhD, and Dr. Scott Semple.
Imaging can provide exquisite details of the fetus. This sagittal half-Fourier acquisition single-shot turbo spin-echo (HASTE) MR image was used for planning further fetal images in other planes, and was taken at the Clinical Research Imaging Center, University of Edinburgh, U.K. Image courtesy of Janet De Wilde, PhD, and Dr. Scott Semple.Cavanagh urges clinical radiologists to consider these points:
- The risk of childhood malignancy following fetal irradiation before the missed menstrual period is probably real, but is likely to be significantly less than the risk from the same dose incurred after the pregnancy itself.
- Common sense and a limited audit in one center suggest that very few patients attending for a high-dose examination will require rescheduling if the 10-day rule is applied to a limited extent.
- Even in the case of inadvertent exposure of an early pregnancy (before or after the first missed menstrual period) to one of the high-dose procedures, the level of risk is not sufficient to justify termination.
"You should consider a limited application of the older 10-day rule to those examinations which fall into the high-dose category," he stated.
The Health Protection Agency provides practical advice about the 10-day rule for high-dose examinations, which result in doses to the uterus of "some tens of milligray," Cavanagh added. For most departments, the only routine examinations approaching this dose level are probably barium enemas and abdominal or pelvic CT, although there are wide variations between departments in the doses resulting from the same examinations.
The guidance was originally issued in 1995 and replaces the previous document (BFCR[95]2), which is now withdrawn.
For further information, he suggests referring to the NHS Choices for Patients platform, the Guidelines for Diagnostic Imaging during Pregnancy from the American Congress of Obstetrics and Gynecology, the Protection of Pregnant Patients During Diagnostic Medical Exposures to Ionizing Radiation from the Health Protection Agency, the RCR and the Society and College of Radiographers. He also recommends the Pre-procedure Pregnancy Checking in Under 16s: Guidance for Clinicians produced by the Royal College of Pediatrics and Child Health.