More than 1,000 subjects recruited for an Italian CT lung cancer screening study stuck with the program through four years of annual follow-up, researchers reported in the Journal of Thoracic Oncology.
Nearly four-fifths of recruited subjects stayed through all four annual screening rounds. And the participants appeared to get something for their persistence, as more than 85% of screen-detected lung cancers were amenable to resection.
On the downside, nearly one-third of participants had a positive result at the initial scan, leading to some unnecessary interventions, while the rate of screen-detected cancers was just 1.5%, according to Dr. Andrea Lopes Pegna, Dr. Giulia Picozzi, and colleagues from Careggi Hospital and Institute for Oncological Study and Prevention in Florence and University Hospital of Pisa (J Thorac Oncol, 22 April 2013).
"Efficacy of screening is weakened by low detection rate and specificity," Pegna and colleagues wrote. "Intervention in benign cases was attributed to not following the protocol. Adhesion to management protocol might lessen surgery for benign lesions," the group wrote.
Lung cancer remains the primary cause of cancer deaths, and just 15% to 20% of symptomatic patients have lung cancers that are amenable to surgery, prompting calls to broaden CT screening efforts to find more cancers in time for curative resection. However, several different randomized screening trials have followed varying protocols and had different results with regard to mortality reduction and screening compliance.
ITALUNG results
In their study, Pegna and colleagues present the final four-year results regarding compliance of subjects recruited in the active arm of the ITALUNG cancer screening trial, including the results of their screens and the results of management protocols for screen-detected suspicious nodules.
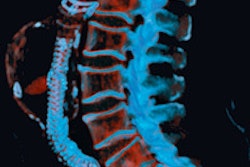
In all, 3,206 individuals at high risk of lung cancer who were invited by mail to participate were asked to undergo low-dose CT (LDCT) scans once per year for four years (n = 1,613) or usual care (n = 1,593). The follow-up protocol included low-dose CT cans, PET scans, and CT-guided fine-needle aspiration biopsy.
The CT scans were performed on one of eight CT scanners among three institutions, including one single-detector scanner, three four-detector-row scanners, two 16-detector-row scanners, and two 64-detector-row machines, all set to 120-140 kV, and 20-43 mAs, with collimation between 3 mm and 0.75 mm, depending on the scanner.
All exams were double read by two experienced readers who had access to all previous scans at each screening round.
Patients underwent repeat screening at six months if detected nodules were 3 mm in diameter or smaller, or three months if they were 3 mm to 5 mm in diameter. For larger nodules or multiple nodules, follow-up CT was performed after one month of antibiotic therapy. PET/CT was sometimes recommended for lesions 8 mm and larger, which in other cases were referred directly for biopsy.
According to the results, a total of 1,406 subjects (87%, 1,035 men and 578 women, 553 former smokers, mean age 60.7 years, mean 42.9 pack years) underwent baseline low-dose CT, and 1,263 (79%) completed four screening rounds.
Low-dose CT was positive in 30.3% of the subjects at baseline and 15.8% in subsequent scans. The researchers detected 21 lung tumors in 20 subjects (1.5% detection) at baseline, and 20 lung tumors in 18 subjects (0.5% detection) in subsequent screening, the group wrote.
"This high recall rate might be because of the radiologist learning curve or reflect characteristics of screened population," Pegna and colleagues wrote.
Lung cancer was diagnosed in 16 of 38 subjects (42%) after evidence of lesion growth at follow-up CT, the group wrote. Ten of 18 prevalent (55%) and 13 of 17 incident (76%) non-small cell cancers were in stage I at detection with CT.
The authors noted "high and sustained compliance" in the active screening arm with 79% of all invited subjects completing four annual rounds. Similar to previous trials, the biggest dropout of active screening subjects (12.8%) came between their agreement to be randomized and the initial scan. Once subjects began, however, they kept going. More than 90% of the subjects who underwent baseline scans completed all four screening rounds.
"The adhesion and compliance rates in the ITALUNG trial might constitute valuable reference terms for future screening programs of lung cancer with low-dose CT involving population-based invitation (by mail or counseling) of subjects at high risk of lung cancer," the authors wrote. "In the active arm of the ITALUNG trial, we observed a low rate of screen-detected lung cancers, which were mostly represented by adenocarcinomas in early stages and were surgically resectable."
The 1.5% prevalence of screen-detected lung cancers in the study is in line with previous observational studies (0.2% to 2.7%) and randomized controlled trials (0.8% to 2.4%), the group wrote. In all, 66% of screen-detected non-small cell lung cancers were in stages IA or IB, in line with previous studies, and 35 of 41 of cancers (85%) in the ITALUNG trial were resectable, again in line with other studies.
"Reduction of the numbers of follow-up or recall LDCT would be valuable, and in our opinion, two basic strategies can be hypothesized," they wrote. "The first concerns recent developments in the efforts to radiologically characterize solitary lung lesions, possibly using CT texture analysis. The second solution entails combination of LDCT with blood or sputum biomarker status, which could independently contribute in identifying subjects with lethal lung cancers appearing as small nodules."
High-risk subjects invited to undergo lung cancer screening do so at lower rates than for comparable breast and colon cancer initiatives, the study team wrote. But once recruited, the participants tend not to drop out.
The results demonstrated that a shared lung cancer screening program based on clinical routine, follow-up CT scans, measurement of mean nodule diameter, FDG-PET and CT-guided fine-needle aspiration biopsy yield high accuracy for preoperative detection of lung cancer, they wrote, adding that the few surgical interventions for benign lesions were associated with protocol violations.