More evidence is needed before radiologists can determine unequivocally that digital breast tomosynthesis (DBT) is ready to replace standard digital mammography, according to a literature review published online in the Breast journal. Fortunately, a number of research studies under way could prove that point.
The findings in the current study offer timely guidance to clinicians about the research needed to support moving DBT into mainstream use, according to authors Dr. Nehmat Houssami, PhD, from the University of Sydney, and Dr. Per Skaane, PhD, from the University of Oslo (Breast, February 18, 2013).
"At present, there is insufficient evidence to justify a change from standard [digital mammography] to DBT; however, the available data strongly support investment in new large-scale population screening trials," Houssami and Skaane wrote.
The researchers reviewed Medline literature that reported on the accuracy of DBT from 2000 through October 2012. They found that published studies of DBT have been relatively small, mostly test-set reader studies or clinical studies that included symptomatic and screen-recalled cases and were enriched with cancers.
Taking these limitations into consideration, Houssami and Skaane summed up the literature findings:
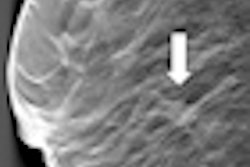
- Two-view DBT has at least equal accuracy when compared to standard two-view digital mammography (craniocaudal and mediolateral oblique [MLO]), whereas one-view DBT (MLO) does not have better accuracy than standard digital mammography.
- Using DBT with standard mammography increases accuracy.
- Better digital mammography accuracy from using DBT may be due to increased cancer detection, reduced false-positive recalls, or both.
- Cancers are equally or more visible on DBT compared to digital mammography.
Initial results from population screening trials also suggest that using DBT with conventional digital mammography may dramatically improve breast cancer detection in mammography screening, but the final outcomes from these trials remain to be seen, according to Houssami and Skaane.
"The evidence and experience so far is that standard 2D mammography plus tomosynthesis improves the accuracy," Houssami told AuntMinnie.com via email. "We feel there is evidence to support more large-scale research in tomosynthesis using 2D plus 3D in breast screening, or to introduce it into clinical practice with careful evaluation of outcomes."
In fact, there are a number of screening trials in progress, Houssami and Skaane wrote, including the following:
- The Oslo Tomosynthesis Screening Trial (OTST), which is part of the Norwegian Breast Cancer Screening Program and is expected to include 18,000 women
- The Malmö Breast Tomosynthesis Screening Trial (MBTST), which will include 15,000 women
- An Italian trial based in Trento and Verona called Screening with Tomosynthesis or Standard Mammography (STORM), early results of which were reported at the European Congress of Radiology in 2012
- A U.K. trial, Tomosynthesis with Digital Mammography (TOMMY), which will include approximately 7,000 women
"Ideally, screening studies should be designed to also demonstrate that by integrating DBT in mammography screening, improved breast cancer detection will ultimately lead to a reduction in interval breast cancers," the researchers concluded.