Belgian researchers have developed a new method designed to sharply reduce the number of clinically irrelevant radiation dose alerts produced by commercial radiation dose-monitoring software.
A team from the department of radiology and medical physics at Antwerp University Hospital in Belgium found that combining acquisition protocol information with CT study descriptions on the RIS led to a 50% drop in radiation dose alerts. All the alerts that were eliminated weren't clinically relevant, but the alerts that remained were.
"Having a well-configured, automated, dedicated software package will reduce workload and offer valuable information regarding your workflow," doctoral student Timo De Bondt told AuntMinnieEurope.com. "Registration of dose opens the gateway to dose reduction."
De Bondt presented the group's results in a session at ECR 2013 in Vienna.
Radiation dose is a perennial concern, and public awareness and governmental concern over radiology practice are bound to increase, according to the researchers. With the goals of alleviating the problem, decreasing radiologists' workload, and improving patient safety, they came up with a new way of working with radiation-dose monitoring software.
','dvPres', 'clsTopBtn', 'true' );" >

Click image to enlarge.
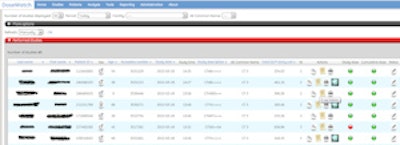
Screenshot of the DoseWatch user interface, depicting an alert triggered by a relatively high radiation dose (red button). All images courtesy of Timo De Bondt.
Radiation dose-monitoring software, in this case DoseWatch (GE Healthcare), which was used in the research project, provides alerts when a CT procedure's dose is deemed too high based on the study description provided by the RIS.
"We found there were some issues with that, mostly because the study description is not specific enough," De Bondt said. "In practice, it contains combinations of several anatomical regions, several acquisitions, and so we calculated alert thresholds based on very heterogeneous data."
Instead, the team gathered information from both the RIS and radiographers, striving to create a more accurate picture of CT dose by utilizing the study description and the acquisition protocol. They then made use of RadLex mapping, a lexicon produced by RSNA for standardizing CT procedures throughout the world to compare radiology practices.
Next, De Bondt and colleagues prepared logical combinations of the study description from the RIS and study protocol from the radiographers to create one RadLex lexicon element, which was then accessed by the dose-monitoring software. The RadLex mapping defines more homogenous groups of procedures, so that the alert triggering level -- two times the median value of dose length product -- is reliable, according to De Bondt.
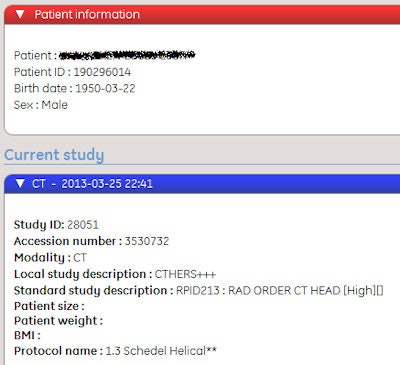 Screenshot of a performed protocol showing a combination of local study description CTBRAIN and acquisition protocol Helical Skull, mapped to RadLex element 213.
Screenshot of a performed protocol showing a combination of local study description CTBRAIN and acquisition protocol Helical Skull, mapped to RadLex element 213.RSNA created a RadLex "Playbook" for CT procedures. In it, a unique identifier is used in information systems to identify the Playbook name. A long version of the name is composed according to the Playbook grammar, for instance: "CT abdomen pelvis lower extremity angiography without then with IV contrast." A short version of the name is used in DICOM header information, such as, "CT ABD PELVIS LE ANGIO W & WO IVCON."
The entry includes a human-readable definition and mappings to RadLex terms that provide components of the Playbook name, such as modality, body part, indications, etc. These mappings are useful in query and data analysis applications, such as dose monitoring, according to RSNA.
In their study over a seven-month period, the researchers mapped 62% of all procedures, which included 10,273 CT scans. When alerts are triggered based on the new grouping of procedures, this new information reduced the amount of alerts from 959 to 466.
Because alert triggers are based on statistical properties of the delivered dose of a procedure, the software groups CT procedures in as homogeneous a way as possible. By combining information from the RIS with input from the performing technician, however, the amount of alerts was reduced by more than 50%, and all were found to have clinical relevance, he said.
Of these 466 alerts, 23 (5%) were not previously reported.
The new alerts could all be attributed to patient or examination-related factors, according to the researchers. Of the 470 alerts (49%) that were no longer reported, none was found to have any clinical relevance.
"The most important thing here is that, in the first place, only the relevant alerts should be triggered," De Bondt said in an interview with AuntMinnieEurope.com.
Limitations
Although the number of alerts was significantly reduced, there was still some heterogeneity within one of the RadLex elements, and only the mapped combinations will generate alerts, he said. So in those cases, no alerts will be issued.
"Of course not all protocols can be mapped, because in practice we will simply find some combinations that make no sense whatsoever," he said, such as a brain CT study description and an ankle CT protocol mapping.
However, using dose management software in combination with these RadLex map procedures will solve the issue of relevant alerts and will reduce workload, De Bondt said.
"We believe in the future we should work on an internationally standardized list grouping CT procedures in this way to be able to compare practices worldwide without any biases introduced," he concluded.



















