Cardiac MR reveals that patients with major depressive disorder have more epicardial fat deposits compared with normal controls -- and, as a result, depressed individuals face a higher risk of heart disease as well -- say researchers from Hannover, Germany.
In their study, Dr. Katja Hüper and colleagues found that patients with major depressive disorder had significantly higher levels of epicardial adipose tissue (EAT) at CMR compared with a group of controls -- and that the levels were highest in patients with a history of chronic depression.
"Increased epicardial adipose tissue may be independently tied to higher cardiac and vascular morbidity in depressed patients, and particularly in patients with a chronic form of this disease," Hüper said in a presentation at RSNA 2012 in Chicago.
Major depressive disorder (MDD) is known to be associated with an increased risk for the development of coronary artery disease, she said.
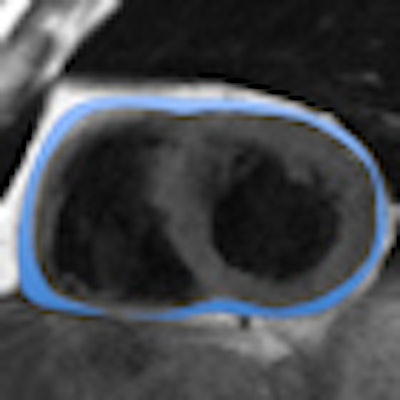
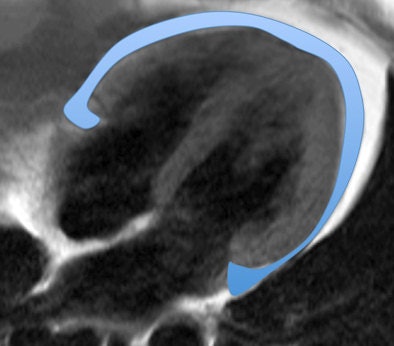 Above, four-chamber view and below, short-axis view of a patient with depression and increased EAT (marked in blue). All images courtesy of Dr. Katja Hüper.
Above, four-chamber view and below, short-axis view of a patient with depression and increased EAT (marked in blue). All images courtesy of Dr. Katja Hüper.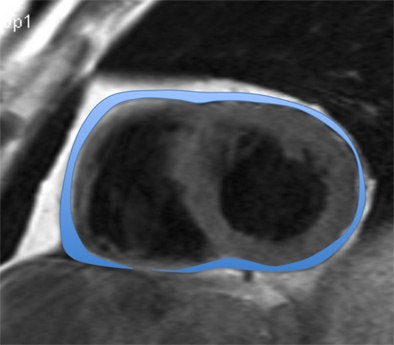
"The reasons for that are not fully understood," Hüper wrote in an email to AuntMinnieEurope.com. It is also known that increased volumes of EAT in the general population are associated with an increased risk for coronary artery disease, she said.
"EAT is a metabolically active visceral fat deposit that via secretion of proinflammatory cytokines is involved in the pathogenesis of coronary artery disease," Hüper explained. "Therefore, we hypothesized that EAT is increased in patients with a major depressive disorder, and that this may contribute to the higher cardiovascular risk in this patient population."
The study aimed to quantify EAT by CMR and compare fat volumes in patients with major depressive disorders versus healthy controls.
Using structured clinical interviews based on the Diagnostic and Statistical Manual of Mental Disorders (DSM volume IV), the researchers grouped patients with major depressive disorder into two groups: 10 patients with chronic MDD (having symptoms that persisted two years or more), and 21 patients with recurrent MDD (history of two ore more depressive episodes). The study also included 25 healthy control subjects.
ECG-gated T1-weighted dark blood turbo spin-echo sequences were acquired in short- and long-axis views on a 1.5-tesla system (Siemens Healthcare). The study team quantified epicardial and paracardial adipose tissue between the atrioventricular plane and the apex using QMass 71 software (Medis).
The researchers also measured concentrations of fasting glucose, cortisol, insulin, tumor necrosis factor-alfa (TNFα), and interleukin-6 in all patients and controls, and they assessed any factors contributing to the metabolic syndrome according to ATP-III criteria. One-way analysis of variance (ANOVA) and chi-square tests were used to sort out differences between the three groups.
The results, adjusted for age and body mass index (BMI), showed that patients with chronic MDD had significantly increased mean EAT volumes (92 ± 7 mL) compared with controls at 69 ± 5 mL (p = 0.016) and patients with recurrent MDD at 66 ± 5 mL (p = 0.006).
"EAT was significantly higher in patients with chronic MDD compared with controls and also compared with recurrent MDD," Hüper said. "The highest volume in the depressive group was 246 mL."
Another type of cardiac fat, paracardial adipose tissue, was also significantly increased in patients with chronic MDD (p = 0.001), Hüper said.
Completing the association between obesity and EAT and depression, the research team found that metabolic syndrome was more frequent in patients with chronic MDD (5/10, 50%) than in controls (2/25, 8%) and patients with recurrent MDD (3/21, 7%) (p = 0.012). Also, tumor necrosis factor TNFα was increased both in patients with recurrent MDD (p < 0.003) and chronic MDD (p < 0.01) as compared with controls.
A main limitation of the study is the small number of patients with major depressive disorder, particularly men. Also there was no evaluation of the effect of therapy "and in particular spot therapy in epicardial fat volumes," Hüper said.
"Epicardial and pericardial adipose tissue was significantly increased in patients with major depressive disorder, and were both associated with increased [inflammatory factor] levels, particularly patients with recurrent depression," she said.
"Epicardial and pericardial adipose tissue were both significantly increased, and therefore we conclude that increased EAT may be independently [associated with] higher cardiac and vascular morbidity in depressed patients," particularly those with chronic depressive symptoms, she said.
EAT is likely to represent an independent risk factor, like obesity and hypertension, that contributes to the higher cardiac morbidity and mortality found in these patients, Hüper said in response to a question from the session moderator.



















