The strong association between hepatic adenomas and the use of oral contraceptive pills and other estrogens is focusing attention on how imaging can help detect and diagnose these rare, benign tumors that occur mostly in women of childbearing age.
MRI is the best tool to characterize hepatic lesions, noted Dr. Maxime Ronot, from the department of medical imaging at Beaujon Hospital and Paris VII University in Clichy, France. In an electronic poster presented at the recent Journées Françaises de Radiologie Diagnostique et Interventionnelle(JFR) congress, she shared her group's experiences of 47 patients in whom MRI classified hepatic adenoma subtypes correctly in 85.1% of cases. Interobserver correlation was excellent, with a kappa value of 0.85, and the technique's sensitivity was 100% and the specificity was 93.3%.
Hepatic adenomas (HCAs) are also known as hepatocellular or liver cell adenomas. Their prevalence in the population is 0.03%, and frequent use of oral contraceptives occurs in around 85% of cases, she explained. The risk increases with the duration of the use of contraceptives and the concentration of estrogens.
 Frequent use of oral contraceptives occurs in around 85% of cases of hepatic adenomas, French researchers said.
Frequent use of oral contraceptives occurs in around 85% of cases of hepatic adenomas, French researchers said.
HCAs are much more frequent in women (sex ratio 9:1), but are also found in men taking anabolic steroids. They are associated with some metabolic conditions, including type I and II glycogen storage disease, tyrosinemia (a genetic disorder characterized by elevated blood levels of the amino acid tyrosine), and galactosemia (a condition in which the body is unable to use/metabolize the simple sugar galactose), and the prevalence of obesity is high. A third of patients have multiple HCAs, according to Ronot.
About 80% of patients are asymptomatic. Cases of HCAs can be accompanied by acute abdominal pain due to bleeding, and heaviness or discomfort of the right hypochondrium. Liver test results are normal in a third of cases. If results are abnormal, the following are observed: cholestasis, and less frequently (one in four cases), a rise in transaminase levels.
HCAs are divided into several subtypes. Classification is based on different pathomolecular signatures for the different subtypes, and establishes a link between mutations and histological and immunohistochemical phenotypes. Consequently, HCAs should no longer be considered as a uniform lesion but as the combination of different entities that share common features and are divided by different morphological aspects, she stated.
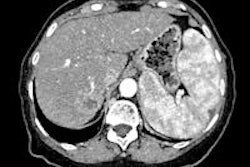
For pathomolecular classification, Ronot explained that researchers from Bordeaux have suggested HCAs are divided into four subtypes, according to the presence or absence of particular mutations: IL-6-gp130-STAT3, hepatocyte nuclear factor 1 alpha (TC1), beta-catenin (Β-catenin) encoded by the CTNNB1 gene, and no specific mutation. Before these various subtypes were identified, the imaging characteristics of HCAs were nonspecific: heterogeneity, and presence of fat and/or bleeding. The various subtypes have been shown to have different morphological properties.
Telangiectatic/inflammatory HCA (tHCA) is the most common form of HCA, accounting for 46-54% of cases, Ronot noted. They correspond to the entity originally described as telangiectatic focal nodular hyperplasia. The physiopathology is linked to mutations of the interleukin 6 pathway (60%), mutations of the IL-6ST gene (which induces oncogene gp130 activity), spontaneous hyperexpression of gp130 (40%), activation of the STAT 3 pathway and induction of hepatocyte proliferation, she added.
Β-catenin activated HCAs (ΒHCA) account for between 8% and 12.5% of HCA cases. The physiopathogeny is linked to mutations that inhibit the CTNNB1 gene, phosphorylation of Β-catenin, nuclear activation of the genes targeted by Β-catenin, and hepatocyte proliferation. The presence of numerous cytological abnormalities is common, and there tends to be neither steatosis nor inflammation. Around 40% of cases occur in men, Ronot estimated.
The specific risk factors for this subtype are glucose storage disease, consumption of male hormones, and familial polyposis. This subgroup is most vulnerable to malignant transformation. Overexpression of >Β-catenin and glutamine synthetase (GS) occurs in the hepatocyte nucleus, she stated.
Nonspecific HCAs account for 5% to 11% of HCA cases. No mutation and no specific morphological properties are associated with this subtype.
ΒHCA and nonspecific HCA imaging is similar to hepatocellular carcinoma (HCC), and they cannot be distinguished from HCC, according to Ronot. Among the signs identified on MRI are intense enhancement in the arterial phase, washout on the portal and late phases, heterogeneous aspect, and the possibility of capsule. Other signs described for ΒHCA are the central scar being poorly defined and hyper-T2 zones being focal and vague. No specific aspect is associated with the nonspecific forms.
Malignant transformation occurs in around 10% of cases. Men account for about half of cases of transformation, and the known risk factors are a diameter great than 5 cm (12%) and Β-catenin activation. Cases of degenerated HCA are hardly ever seen with sHCA, and the condition cannot be diagnosed before surgery on the basis of any clinical or radiological information, she stressed.
In practice, the usefulness of a biopsy depends on the subtype, as shown by the MRI examination. For sHCA, a biopsy is not indicated for diagnosis, but can be useful in doubtful cases where a tHCA with steatosis is suspected. For tHCA, a biopsy is not indicated for diagnosis, but may be useful for assessing Β-catenin status. For the two other subtypes, a biopsy is indicated to rule out HCC and assess Β-catenin status, concluded Ronot.
Acknowledgment: The original French text of this JFR e-poster was translated by Syntacta Translation & Interpreting, Swindon, U.K.