MRI can be a reliable and reproducible tool in providing clinical information on placental invasion -- placenta accreta, increta, or percreta -- but its diagnostic value still depends crucially on observers' experience, Swiss researchers have found.
Placental implantation disorders are classified as abnormal localization and abnormal attachment. Abnormal placental localization occurs in 1 out of 250 pregnancies, whereas abnormal placental attachment occurs in 1 in 5,000, according to Dr. Leonor Alamo, from the department of radiology at Centre Hospitalier Universitaire Vaudois in Lausanne, Switzerland, and colleagues.
The three kinds of attachment abnormalities -- placenta accreta, increta, and percreta -- represent a spectrum of placental adhesive disorders, with increasing severity.
"These implantation disorders are a significant cause of maternal morbidity and mortality," Alamo and colleagues wrote (European Journal of Radiology, 26 September 2012, article in press). "Their prevalence is currently on the rise because of the growing percentage of older pregnant women and those with previous abortions and/or caesarean sections."
Screening ultrasound at 18-20 weeks of pregnancy is the routine diagnostic imaging method used to evaluate the placenta, but it may be inconclusive or equivocal in cases of a difficult visualization of the placenta due to the patient's body habitus or a posterior placental implantation, they added.
MRI is increasingly being used for confirmation of suspected placental anomalies or in cases of equivocal ultrasound findings. However, the MR signs may be subtle and difficult to detect, especially if the radiologist has limited experience. Alamo and colleagues sought to determine the diagnostic value of specific MR features for detecting suspected placental invasion according to the radiologists' working experience.
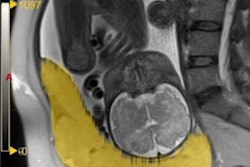
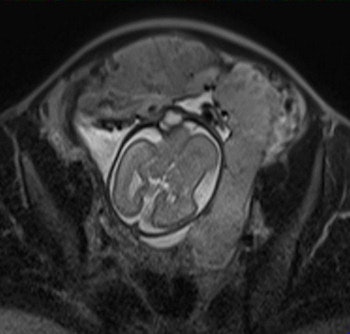 Axial T2-weighted single-shot fast spin-echo MR image shows an irregular outer uterine contour with discontinuity of the T2-hypointense myometrial layer in the anterior uterine segment. All images courtesy of Dr. Leonor Alamo.
Axial T2-weighted single-shot fast spin-echo MR image shows an irregular outer uterine contour with discontinuity of the T2-hypointense myometrial layer in the anterior uterine segment. All images courtesy of Dr. Leonor Alamo.Their retrospective study included 25 pregnant women (mean age 35.16) -- 12 with histopathologically proven placental invasion and 13 without to act as a control -- who were investigated by prenatal MRI without IV contrast at three hospitals using three different 1.5-tesla MRI units (Magnetom Symphony, Siemens Healthcare; Intera, Philips Healthcare; Signa, GE Healthcare). The women underwent MR imaging between June 2007 and December 2009 after obstetrician referral for suspected placental invasion upon standard pregnancy ultrasound exams. The MRI protocols were similar and included T1-weighted volume interpolated gradient-echo MR sequences in the sagittal and axial plane, single-shot fast spin-echo T2-weighted MR sequences, and true fast imaging with steady-state precession in the axial, sagittal, and coronal planes.
Two senior radiologists with more than five years of practical experience in abdominal MRI and two junior radiologists with less than three years of abdominal MRI experience blindly and independently reviewed MR exams for six previously defined MR features described in the literature as useful for predicting placental invasion. The features included dark intraplacental bands on T2-weighted images, a focally interrupted myometrial border, heterogeneous intraplacental signal intensity, abnormal uterine bulging, "tenting" of the bladder, and infiltration of the adjacent pelvic organs.
Overall sensitivity and specificity for placental invasion was 90.9% and 75.0%, respectively, for seniors and 81.8% and 61.8%, respectively, for juniors. The best single MR feature indicating placental invasion was T2-hypointense placental bands, followed by focally interrupted myometrial border, infiltration of pelvic organs, and tenting of the bladder.
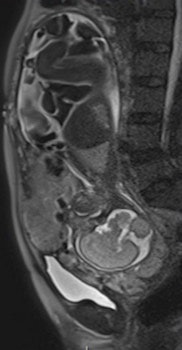
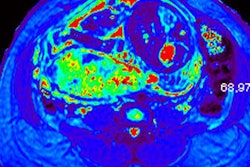
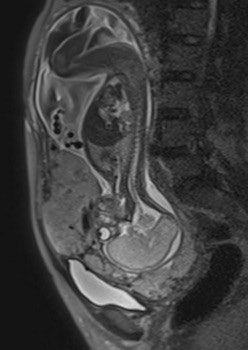 Sagittal T2-weighted single-shot fast spin-echo MR images show the placenta previa and evidence focal bulgings of the anterior uterine wall. The signal intensity of the placenta is heterogeneous, with presence of T2-hypointense placental bands. Observe the discontinuity of the myometrial layer, extending beyond the uterine serosa.
Sagittal T2-weighted single-shot fast spin-echo MR images show the placenta previa and evidence focal bulgings of the anterior uterine wall. The signal intensity of the placenta is heterogeneous, with presence of T2-hypointense placental bands. Observe the discontinuity of the myometrial layer, extending beyond the uterine serosa.The kappa values for interobserver agreement for detecting placental invasion were substantial (0.64) for seniors and moderate (0.41) for juniors. Seniors detected placental invasion and depth of infiltration with significantly higher diagnostic accuracy than juniors.
The most important difference in sensitivity and specificity of both groups was found in detecting a focally interrupted myometrial border (sensitivity of 90.0% for seniors versus 81.8% for juniors and specificity of 62.4% for seniors versus 42.6% for juniors).
"Although junior readers have a higher sensibility in the detection of abnormal uterine bulging than seniors (77.25 versus 59.1), their specificity was very low compared to that obtained by seniors readers (13 for juniors versus 41.3 for seniors)," the researchers wrote. "According to our data, a focally interrupted myometrial border seems to be the MR feature that reveals the most important differences between junior and senior readers."
Senior readers also showed significantly better diagnostic accuracy than junior readers in evaluating the presence of dark intraplacental bands on T2-weighted images, a focally interrupted myometrial border, and abnormal uterine bulging. However, the researchers found no significant difference regarding the detection of heterogeneous intraplacental signal intensity. The senior readers did score better in predicting placental invasion though.
Risk factors for placental invasion
Other than the previously mentioned advanced age of some pregnant women, the increasing rate of uterine surgery, and caesarean sections, another well-known risk factor is placenta previa. The incidence of placenta accreta has been reported to be as high as 5% in women with a previous caesarean section and increases up to 67% in the presence of both placenta previa and multiple previous caesarean sections.
Placenta previa was present in all but one of the 12 women with proven placental infiltration, and three of them also had a previous caesarean delivery, Alamo's team wrote.
Nondetected abnormalities in placental attachment may produce intense hemorrhages at delivery, which often require emergency postpartum hysterectomy and are also the cause of high morbidity and even mortality for the mother and fetus.
"Prenatal identification of placental disorders is therefore crucial in order to plan delivery and to reduce complications," the researchers wrote.
In normal patients, the uterus presents as an inverted pear-shape organ. At MRI, the normal placenta appears as a soft-tissue structure, located along the uterine walls, with variable morphology and homogeneous, intermediate, signal intensity on T2-weighted images. In Alamo's study, T2-hypointense placental bands, a focally interrupted myometrial border, infiltration of the pelvic organs, and tenting of the bladder proved to be the best signs of predicting placental invasion.
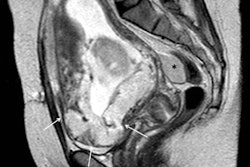
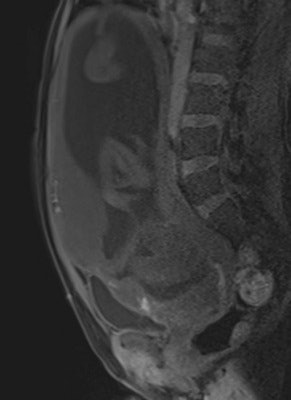 Sagittal T1-weighted volume interpolated gradient-echo MR image evidences focal hyperintense signal intensity of the placenta, compatible with recent hemorrhages.
Sagittal T1-weighted volume interpolated gradient-echo MR image evidences focal hyperintense signal intensity of the placenta, compatible with recent hemorrhages."The combination of these four imaging features shows a stepwise multiple regression coefficient of 0.36. Our data suggest that this 'gold combination' increases the specificity of MRI and may enable a reliable detection of placental implantation disorders," they wrote.
Alamo and colleagues concluded that medical practices face an increased prevalence of placental adhesive disorders in the near future because of a higher mean maternal age and an increase of uterine surgery procedures.
"Today, MRI of the placenta has become a complementary method to [ultrasound] for patients at risk and in selected, equivocal cases. Different MR features have been described in association with placental disorders, but our results suggest that their recognition and correct interpretation very much depend on readers' experience," they wrote. "Therefore, we consider that placental MRI should be performed in selected reference centers in order to guarantee the radiological level of experience required for the correct diagnosis."
The researchers acknowledged some limitations to their study: They had a reduced number of cases of placenta percreta and, thus, the MR features "tenting" of the bladder and infiltration of the adjacent organs could only be evaluated in a few patients, so their results need to be interpreted with caution. Also, this was a retrospective study involving three different hospitals, with different MRI units and protocols, and, therefore, the results should be confirmed by larger, more homogeneous trials.