Combining digital breast tomosynthesis (DBT) with mammography is just as good as standard two-view mammography, Italian researchers report. In fact, the combination was superior when it comes to recognizing benign lesions.
DBT has been creeping up on mammography for a while in terms of taking over its turf, and at the ECR in March it was proclaimed DBT will replace mammography in 10 years. Slowly the scientific literature has started to catch up. Previous retrospective clinical performance studies on DBT have taken two different approaches: whether DBT, in one or two views, could replace standard mammography; or to test DBT as a new diagnostic tool to be used as an adjunct to 2D mammography to obtain additional information.
The Italian study was published online on 14 September in European Radiology. Lead author Dr. Gisella Gennaro, a medical physicist from the Veneto Institute of Oncology in Padua, and colleagues compared the clinical performance of standard two-view digital mammography with the combination of one-view tomosynthesis (mediolateral oblique) and one-view mammography (craniocaudal). A multiple-reader, multiple-case receiver operating characteristics (ROC) experiment was performed, and clinical performance was reported in terms of area under the ROC curve (AUC), sensitivity, and specificity.
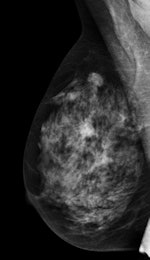
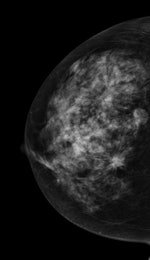
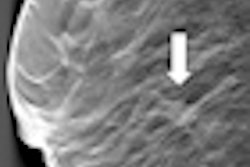
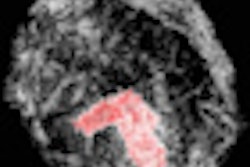
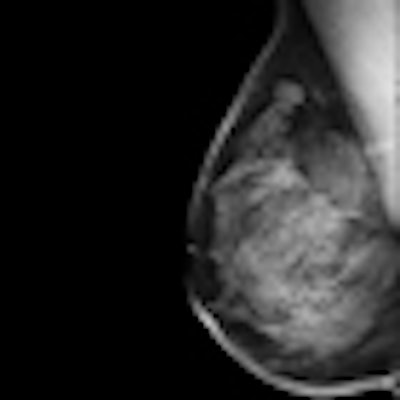
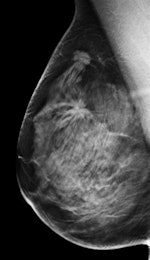 Left: Mediolateral oblique view of a patient with two malignant masses (invasive ductal carcinomas) using mammography. Center: Same patient viewed via craniocaudal mammography. Right: Same patient viewed on DBT. The spicules and tumor structures are better depicted by DBT. Copyright Dr. Gisella Gennaro.
Left: Mediolateral oblique view of a patient with two malignant masses (invasive ductal carcinomas) using mammography. Center: Same patient viewed via craniocaudal mammography. Right: Same patient viewed on DBT. The spicules and tumor structures are better depicted by DBT. Copyright Dr. Gisella Gennaro."Manufacturers are now progressively moving from prototype systems to clinical products, and exposure control is being optimized, allowing the acquisition of a DBT view at the same dose as a single mammography view," the authors noted. "This would permit use of a combined technique, like the one proposed in this work, at the same dose level as the reference standard (two-view digital mammography), with some benefits in terms of clinical performance, or, alternatively, use mediolateral oblique-view DBT alone at comparable performance to that of two-view mammography, but at half the breast dose."
Six breast radiologists reviewed images from 250 patients who underwent bilateral mammography and DBT imaging. Mammography and DBT images with the adjunct of the craniocaudal mammography view from 469 breasts were evaluated and rated independently by six readers.
The combined technique was found to be noninferior to standard two-view mammography in mean AUC (difference: +0.021; 95% confidence interval: -0.011, +0.052), but was not statistically significant for superiority. The combined technique had equivalent sensitivity to standard mammography (76.2% versus 72.8%) and equivalent specificity (84.9% versus 83.0%). Specificity for benign lesions was significantly higher with the combination of techniques versus mammography (45.6% versus 36.8%).
Adding craniocaudal-view mammography to mediolateral oblique DBT improves overall clinical performance compared with DBT alone, moving the lower confidence limit of the mean AUC difference with standard mammography closer to zero, Gennaro and colleagues wrote.
"Demonstration of superiority would require the entire confidence interval of the AUC difference to stay above zero; the trend toward superiority suggests that the additional information gained by adding a craniocaudal view mammography to mediolateral oblique DBT may have a positive effect on clinical performance compared with mammography," they noted.
Because DBT is still a fairly new technology, radiologists don't have much experience using it. "At this early stage in the use of DBT, it might be prudent to add a craniocaudal mammography view to mediolateral oblique DBT, both to increase radiologists' confidence with the new technique and to recover possible information missing from DBT because of limited experience and possible exclusion of cancers from single-view mediolateral oblique positioning of DBT," the authors explained.
In addition, using DBT with a single complementary mammography view could allay radiologists' fears about the detection of subtle microcalcifications -- current studies show DBT's sensitivity for detecting calcifications is lower than mammography's. The combined technique proposed in Gennaro's study could aid calcification detection and help train radiologists to recognize and properly rate calcifications on DBT images.
In terms of specificity, the technique did not show statistically significant differences when the standard definition of specificity was applied, but variability was much lower than observed when comparing mediolateral oblique DBT alone with standard two-view mammography.
"Looking at specificity using the two separate definitions proposed for benign lesions and normal cases, a significant benefit was shown for benign lesions in terms of detection and characterization using DBT plus mammography," Gennaro and collagues wrote. "This result suggests that a combination of DBT and mammography might reduce the recall rate for benign lesions compared with mammography alone."
When breasts without lesions were considered, specificity with the combined technique was slightly lower than mammography, which may be due in part to the process of truth establishment for breasts with and without lesions, which was based on standard techniques (mammography and ultrasound) but not on DBT, according to the authors.
"It is possible that a benign lesion was not seen by mammography and that the breast was therefore considered normal, but the benign lesion appeared on DBT because of the better separation of superimposed breast tissue when viewing individual tomographic planes," they stated. "Another possible reason is that, despite readers knowing that DBT reduces superimposed anatomical noise, overlapping tissues observed in the craniocaudal mammography were not disregarded because of readers' greater confidence with the established technique."
As usual, dose is a concern. Earlier studies on tomosynthesis limited the number of views to one mainly for dose constraints. Those studies (like this one) used prototype equipment for DBT acquisition, often without automatic exposure control, choosing a sweep angle and a number of projections as large as possible, while keeping the total dose within limits defined for standard two-view mammography.