Conducting a CT dose survey is essential for understanding and analyzing practice, and the mean values from these surveys are useful to compare with national or even international diagnostic reference levels (DRLs) to facilitate benchmarking and ultimately optimization of dose, concludes a new Australian study published online by the British Journal of Radiology on 27 July.
"There is greater awareness and utilization of tools such as DRLs to reduce and manage dose," noted lead author Zoe Brady, PhD, radiation safety officer and medical physicist at the Alfred radiology department in Melbourne, Australia. "Assessing local practice is essential for proactive optimization and increasing dose awareness among staff."
![Chest CT of 8-day-old girl with respiratory distress (80 kV, 51 average effective mAs, CTDIvol = 2.3 mGy, DLP [dose length product] = 33 mGy cm, E[effective dose] = 1.1 mSv. CT was performed to exclude congenital lung abnormalities because of family history and small volume lungs. Image shows ground glass opacity and septal lines consistent with respiratory distress syndrome. In all four figures, CTDIvol and DLP are expressed in terms of the 16 cm CT dosimetry phantom; these should be divided by approximately two to be expressed in terms of the 32 cm CT dosimetry phantom. Effective dose was calculated from DLP using conversion coefficients specific to this scanner and using the International Commission on Radiological Protection Publication 103 definition of effective dose. All images courtesy of Zoe Brady, PhD.](https://img.auntminnieeurope.com/files/base/smg/all/image/2012/08/ame.2012_08_15_08_57_30_715_2012_08_15_pediatrict_CT_pic1.png?auto=format%2Ccompress&fit=max&q=70&w=400) Chest CT of 8-day-old girl with respiratory distress (80 kV, 51 average effective mAs, CTDIvol = 2.3 mGy, DLP [dose length product] = 33 mGy cm, E[effective dose] = 1.1 mSv. CT was performed to exclude congenital lung abnormalities because of family history and small volume lungs. Image shows ground glass opacity and septal lines consistent with respiratory distress syndrome. In all four figures, CTDIvol and DLP are expressed in terms of the 16 cm CT dosimetry phantom; these should be divided by approximately two to be expressed in terms of the 32 cm CT dosimetry phantom. Effective dose was calculated from DLP using conversion coefficients specific to this scanner and using the International Commission on Radiological Protection Publication 103 definition of effective dose. All images courtesy of Zoe Brady, PhD.
Chest CT of 8-day-old girl with respiratory distress (80 kV, 51 average effective mAs, CTDIvol = 2.3 mGy, DLP [dose length product] = 33 mGy cm, E[effective dose] = 1.1 mSv. CT was performed to exclude congenital lung abnormalities because of family history and small volume lungs. Image shows ground glass opacity and septal lines consistent with respiratory distress syndrome. In all four figures, CTDIvol and DLP are expressed in terms of the 16 cm CT dosimetry phantom; these should be divided by approximately two to be expressed in terms of the 32 cm CT dosimetry phantom. Effective dose was calculated from DLP using conversion coefficients specific to this scanner and using the International Commission on Radiological Protection Publication 103 definition of effective dose. All images courtesy of Zoe Brady, PhD.The researchers compared average dose values at the Royal Children's Hospital (RCH) in Melbourne with international DRLs for common pediatric CT examinations. They found the use of 80 kV for both chest and abdomen/pelvis imaging in children younger than 5 years old leads to a significant dose saving, but conceded there is potential for dose optimization by reducing scan lengths for body examinations for children older than 5 years old. The plan now is to review these protocols to determine whether there is appropriate justification for the extended scan lengths.
Furthermore, the reference mAs values for chest imaging must be justified, particularly relative to the abdomen/pelvis examination values for the same age groups, according to Brady. Because of the inherent contrast in the chest and lack of attenuating tissue, it was expected that these values might be lower for chest examinations than for abdomen/pelvis examinations, but in fact in the older age group they were found to be higher.
"We have recently upgraded to a dual-energy CT scanner and we intend to investigate and lower protocol parameters using a similar optimization method. We now have the added benefit of structured dose reporting, which helps automate the task of data collection," she pointed out in an email. "The results from this original study provide us with a useful baseline for comparison. Overall, we have greater control and understanding of the potential for dose reduction."
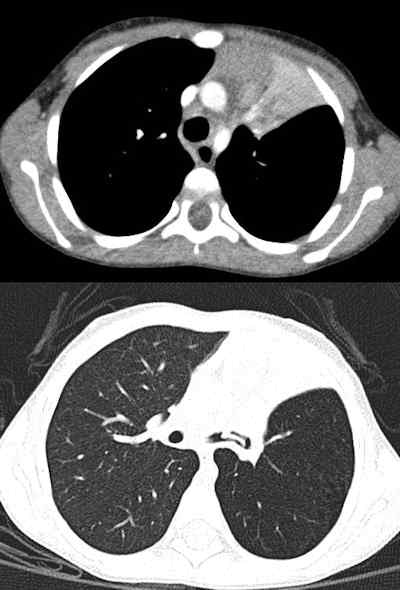 Chest CT of 3-year-old boy performed because of chronic cough and left upper lobe (LUL) collapse (80 kV, 53 average effective mAs, CTDIvol = 2.5 mGy, DLP = 58 mGy cm, E = 1.9 mSv). Images show normal vascular enhancement and LUL collapse in upper image with mediastinal window settings and foreign body in left main bronchus in the lung window images.
Chest CT of 3-year-old boy performed because of chronic cough and left upper lobe (LUL) collapse (80 kV, 53 average effective mAs, CTDIvol = 2.5 mGy, DLP = 58 mGy cm, E = 1.9 mSv). Images show normal vascular enhancement and LUL collapse in upper image with mediastinal window settings and foreign body in left main bronchus in the lung window images.The authors carried out a retrospective audit of patient records for pediatric CT brain, chest, and abdomen/pelvis exams. Demographic information, exam parameters, and dose indicators (volumetric CT dose index [CTDIvol] and dose-length product [DLP]) were collected for 220 patients: 100 for CT brain exams and 60 for each of the CT chest and abdomen/pelvis exams. Local DRLs (LDRLs) were derived from mean survey values and the effective dose was estimated from DLP values. The normalized CTDIvol values, mAs values, and scan length were assessed to better identify parameters that could be optimized.
All scans were performed on a Sensation 16 multidetector CT (MDCT) scanner with a Straton x-ray tube (Siemens Healthcare) utilizing automatic tube current modulation (CARE Dose4D, Siemens). The gender, age, parameters used (tube potential, time per rotation, detector configuration, beam collimation, pitch, effective mAs), and dose indicators were recorded for each patient.
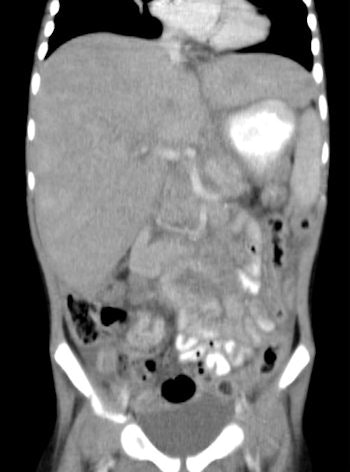 CT of abdomen and pelvis in 3-year-old girl was performed to reassess recurrence of neuroblastoma (80 kV, 70 average effective mAs, CTDIvol = 3.2 mGy, DLP = 112 mGy cm, E = 2.6 mSv). Coronal CT of abdomen shows para-aortic mass.
CT of abdomen and pelvis in 3-year-old girl was performed to reassess recurrence of neuroblastoma (80 kV, 70 average effective mAs, CTDIvol = 3.2 mGy, DLP = 112 mGy cm, E = 2.6 mSv). Coronal CT of abdomen shows para-aortic mass.The LDRLs across all age categories were 18-45 mGy (CTDIvol) and 250-700 mGy cm (DLP) for brain examinations; 3-23 mGy (CTDIvol) and 100-800 mGy cm (DLP) for chest examinations; and 4-15 mGy (CTDIvol) and 150-750 mGy cm (DLP) for abdomen/pelvis examinations. Effective dose estimates were 1.0-1.6 mSv, 1.8-13.0 mSv and 2.5-10.0 mSv for brain, chest, and abdomen/pelvis examinations, respectively. The RCH mean CTDIvol and DLP values were similar to or lower than international DRLs.
In the future, it may be worthwhile deriving local DRLs for common protocols based on clinical indication and/or weight, and this may result in narrower ranges for the scan lengths and allow more directed LDRLs, the authors stated. However, many factors need to be considered when comparing local doses with DRLs and the dose indicators need to be properly defined in terms of the CT dosimetry phantom used and the type of examination.
 CT of abdomen and pelvis in 15-month-old girl was performed for follow-up of neuroblastoma (80 kV, 57 average effective mAs, CTDIvol = 2.6 mGy, DLP = 69 mGy cm, E = 1.6 mSv). Image displayed is coronal reconstruction, which shows partly calcified mass in left abdomen. Ureteric stent was noted in bladder.
CT of abdomen and pelvis in 15-month-old girl was performed for follow-up of neuroblastoma (80 kV, 57 average effective mAs, CTDIvol = 2.6 mGy, DLP = 69 mGy cm, E = 1.6 mSv). Image displayed is coronal reconstruction, which shows partly calcified mass in left abdomen. Ureteric stent was noted in bladder.This study demonstrates that using several quantities isolates the influence of each factor on dose and enables the identification of protocol parameters and areas of operator technique that can be optimized, they concluded.