PET cannot rule out malignancy in pulmonary nodules less than 12 mm on expiratory CT, and melanoma patients with PET-negative pulmonary nodules less than 12 mm require further investigation, a new Austrian study has found.
"Additional tests are recommended for melanoma patients who present with one or more PET-negative lung nodules that measure less than 12 mm on expiratory CT," noted lead author Dr. Marius E. Mayerhoefer, PhD, from the department of radiology at the Medical University of Vienna. "This strategy may help avoid understaging of the disease and thus the selection of an inappropriate form of therapy. Respiratory gating, which is presently not a standard procedure for PET image acquisition, may improve the sensitivity of PET for pulmonary lesion detection."
In patients with malignant melanoma, one of the most important prognostic factors is the presence of metastases, and patients with distant metastases have a poor prognosis, he explained in an article published online by European Radiology on 1 June. Spread to the lungs, for instance, is associated with a one-year survival rate of only 53%, and because these patients might benefit from surgical excision of pulmonary metastases in terms of survival, early detection is of the utmost importance.
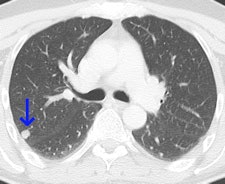
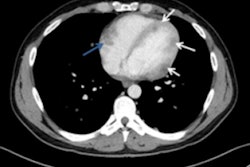
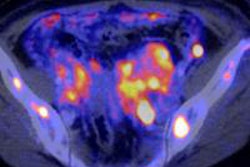
 This 62-year-old melanoma patient has a 10-mm metastasis in the right upper lobe. The CT image (left) failed to show increased tracer uptake on the F-18 FDG PET image (right). All images courtesy of Dr. Marius Mayerhoefer.
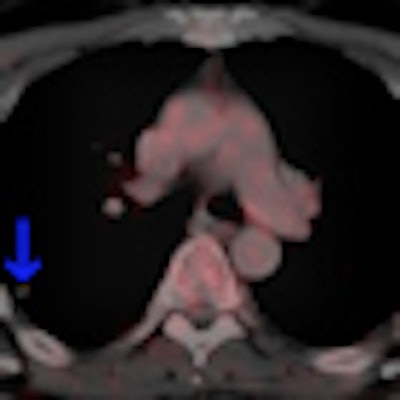
This 62-year-old melanoma patient has a 10-mm metastasis in the right upper lobe. The CT image (left) failed to show increased tracer uptake on the F-18 FDG PET image (right). All images courtesy of Dr. Marius Mayerhoefer.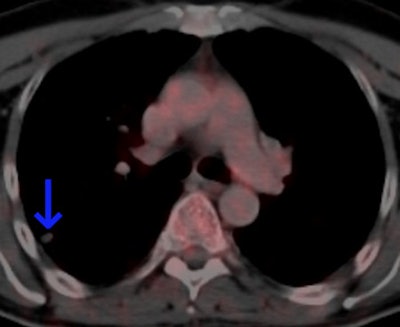 The same patient as seen with the fused color-coded PET/CT image.
The same patient as seen with the fused color-coded PET/CT image.F-18 FDG PET can help in the workup of pulmonary nodules because it reflects the tissue glucose metabolism, which is elevated in most malignant lung lesions. But mainly due to its limited spatial resolution, the sensitivity of PET for detecting pulmonary metastases is only moderate: In melanoma patients, it is between 57% and 70%, according to Mayerhoefer.
"CT can reliably detect even very small pulmonary nodules, owing to the high contrast between the nodules and the surrounding lung tissue, and thus has a higher sensitivity than PET for the detection of pulmonary melanoma metastases," he stated. "However, CT cannot reliably distinguish between benign and malignant lesions and is therefore less specific. The introduction of PET/CT has improved the situation in this regard."
The authors sought to investigate the dependence of PET sensitivity on the size of pulmonary melanoma metastases, and to determine at which size a pulmonary metastasis can be expected to be PET-positive. They wanted to help clinicians to more accurately determine the subgroup of patients who require further evaluation for a definite staging.
All patients with histologically proven cutaneous melanoma who were referred to the local PET/CT center for staging or follow-up between January 2008 and June 2011, were included in the retrospective study. Whole-body F-18 FDG PET/CT was performed using a Biograph 64 TruePoint PET/CT system (Siemens Healthcare). Glucose levels were measured before the examination, with a cut-off limit of 8 mmol/L (150 mg/dL). Imaging was performed 50-60 minutes following intravenous administration of 300 MBq of F-18 FDG, and an intravenous injection of 100 mL of a tri-iodinated, nonionic contrast medium (Iomeron 300, Bracco) at a rate of 2 mL/sec, followed by a 50-mL saline flush.
CT images of the lungs were reconstructed with a lung kernel (B60f). PET images were reconstructed using the iterative TrueX algorithm (Siemens Healthcare).
Of 183 patients with proven cutaneous melanoma who underwent F-18 FDG PET/CT between January 2008 and June 2011 at the institution, 38 patients (18 women and 20 men; mean age 62.0 ± 14.7 years) fulfilled the authors' criteria for participation in the study. A total number of 181 lung nodules that were rated as melanoma metastases according to the mixed standard of reference were found in these patients. Of these 181 metastases, 132 (72.9%) met one criterion for malignancy, 47 (26%) met two criteria, and two patients (1.1%) met three criteria. In those nodules that were classified as metastases on the basis of their growth rate, the mean doubling time was 94.2 ± 58.8 days (range 30-288 days). In those lesions that were verified by a positive PET with an SUVmax of at least 2.5, the mean SUVmax was 10.4 ± 10.1 (range 2.6-59.6).
Overall, PET was true-positive in 86 nodules and false-negative in 95 nodules, providing a lesion-based overall sensitivity of 47.5% (95% confidence interval [CI]: 0.40 to 0.55). Twenty-nine patients were true-positive for the presence of lung metastases on PET (i.e., at least one lung metastasis was PET-positive), and nine were false-negative, providing a patient-based sensitivity of 76.3 % (95% CI: 0.62 to 0.90).
"Our results clearly show that, in melanoma patients, a negative PET scan does not rule out malignancy in pulmonary nodules of less than 12 mm, despite the use of modern PET/CT equipment. This size threshold is higher than we had expected, and may in part be explained by the fact that the CT images of PET/CT examinations were obtained in expiration for the sake of optimal coregistration with PET; had CT been performed in inspiration, the threshold may possibly have been lower by about 1 mm. In the present study, some 4- to 5-mm lesions showed an increased tracer uptake. However, the vast majority (92.1%) of pulmonary melanoma metastases in this group (4-5 mm) was PET-negative," they concluded.
The group's future research will focus on the effect of different PET image reconstruction algorithms on detecting small malignant lung nodules, and on an improved assessment of mediastinal invasion of lung cancer by means of hybrid imaging techniques.