Outsourcing after-hours CT coverage to a teleradiology services provider can be achieved with a low error rate, the authors of a study published online in the European Journal of Radiology have found.
In a retrospective study of the after-hours teleradiology reports of more than 1,000 patients over a five-month period, a research team led by Dr. Joachim Hohmann of the University College Hospital in London found that their teleradiology services provider only had a 0.8% rate of major interpretation errors. That rate was also lower than the 1.6% to 24% rate other studies have found from preliminary in-house staff reports, noted the researchers.
The research group sought to evaluate the level of agreement between after-hours out-sourced teleradiology reports with the reports of an in-house panel. They also followed up the patients in which there were serious disagreement to determine which of the reports had the accurate diagnosis (Eur J Radiol, May 17, 2012).
Between December 2009 and April 2010, 1,028 patients had imaging exams performed between 7 p.m. and 8 a.m. at a central London university hospital. These patients received an average of 1.42 imaging exams, including an aggregate of 473 head CT studies, two CT orbita, 19 CT facial bones, eight CT neck, 155 CT chest, 362 CT abdomen and pelvis, seven CT pelvis only, 54 CT spine, eight CT extremities, and 11 CT angiograms.
All studies were interpreted by Imaging Partners Online (IPO), which has offices in the U.K. and Australia. Reporting radiologists at IPO were all accredited consultants with General Medical Council (GMC) specialist registration, according to the authors.
Images were sent to the teleradiology services provider along with previous exams and clinical information. Reports were due back within one hour and were sent by secured email. If necessary, the reporting radiologists were able to consult over the telephone with referring physicians and on-site radiographers.
The next morning, a panel composed of two consultant radiologists, one fellow, and two registrars reviewed the cases, blinded to the initial teleradiology report. The consultants were the final decision-makers on the cases, and rated their assessment of agreement with the initial report on a five-point scale, including 1 (definite omission or misinterpretation with unequivocal potential for serious morbidity or threat to live), 2 (definite omission or interpretation of finding with strong likelihood of moderate morbidity but not threat to life), 3 (clinical significance of disagreement is debatable or likelihood of harm is low), 4 (disagreement over style and/or presentation of the report including failure to describe clinically insignificant features), and 5 (no disagreement).
Agreement between teleradiology reports and panel reports
- Category 5: 811 patients (78.9%)
- Category 4: 164 patients (15.9%)
- Category 3: 40 patients (3.9%)
- Category 2: 13 patients (1.3%)
- Category 1: 0 patients
Detailed follow-up for six months was performed on the 13 patients in category 2 (definite omission or interpretation of finding with strong likelihood of moderate morbidity but not threat to life). In these cases, eight (0.8%) turned out to be incorrect teleradiology reports.
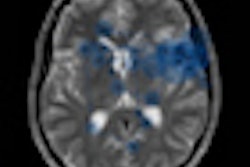
These misses included one intracerebral abscess, one new occipital infarction, two pulmonary embolism, one coeliac axis thrombosis, and one anastomotic leak. In addition, the teleradiology service incorrectly diagnosed appendicitis in which there was a clear appearance of a pancreatitis, according to the authors.
While the patients with the intracerebral abscess, the coeliac axis thrombosis, and the pancreatitis died during the follow-up period, the authors said this was more likely due to the severity of the disease rather than the initially false report.
For its part, the in-house panel incorrectly diagnosed two cases (0.2%), including a bilioma and a missed perforating appendicitis. The correct diagnosis remained unclear in the remaining three category 2 patients.
The team also noted the benefits of teleradiology for emergency after-hours examinations. Studies were usually received within one hour after finishing the exam and the workflow was also considered to be smooth, according to the researchers.
"As a consequence of this along with the relatively small number of misinterpreted findings, the overall satisfaction with the service was high by the referring physicians," they stated.
The researchers acknowledged a number of limitations of their study, including the evaluation of only one teleradiology services provider.
"However, if all reporting radiologists are officially accredited and registered consultants and if they are equipped with state-of-the-art technology, as in our study, this might not be an issue," the authors wrote.
The researchers also said they did not calculate the exact times needed for reports and that three cases remained unclear even after the follow-up period.
Nonetheless, the authors concluded, "The results of the present study support the use of an outsourced after-hours teleradiology reporting service regarding the issue of quality concerns of such an attempt."