MRI is proving useful in the prenatal diagnosis and evaluation of complex fetal thoracic pathologies, and is invaluable in assisting surgical planning where complicated anatomical abnormalities exist, Irish radiologists have discovered.
"Fetal MRI plays an ever-increasing complementary role to prenatal ultrasound in the evaluation of the fetus with suspected abnormalities," noted Dr. Sara Hayes, from Cork University Hospital, in a presentation at the recent RSNA congress. "Its role includes confirming the presence of abnormal pathology, defining its full extent, aiding in its characterization, and demonstrating other associated abnormalities. MRI can also aid in the planning of postnatal surgery."
MRI examinations should be avoided during the first trimester, and gadolinium-based contrast is relatively contraindicated in pregnancy. At Cork, the use of B channel torso phased array coils and supine positioning is preferred, and sedation is not used routinely.
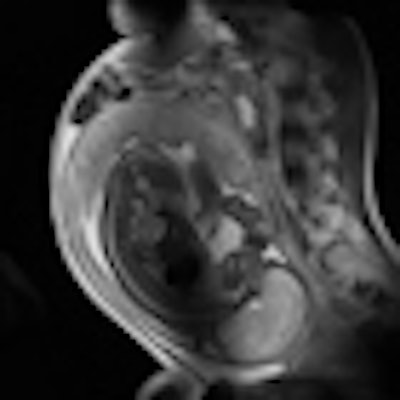
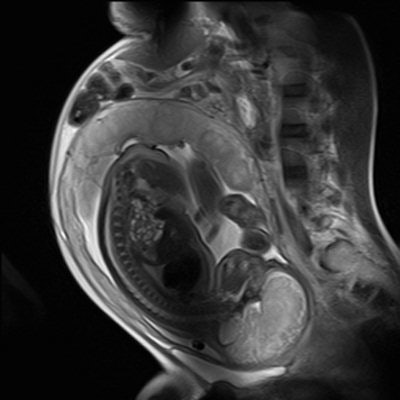 There is no firm evidence that clinical MR procedures during pregnancy produce adverse effects, the experts say. This sagittal half-Fourier acquisition single-shot turbo spin-echo (HASTE) image was used for planning further fetal images in other planes, and was taken at the Clinical Research Imaging Center, University of Edinburgh. Image courtesy of Janet De Wilde, PhD, and Dr. Scott Semple.
There is no firm evidence that clinical MR procedures during pregnancy produce adverse effects, the experts say. This sagittal half-Fourier acquisition single-shot turbo spin-echo (HASTE) image was used for planning further fetal images in other planes, and was taken at the Clinical Research Imaging Center, University of Edinburgh. Image courtesy of Janet De Wilde, PhD, and Dr. Scott Semple.The fetal trachea is filled with amniotic fluid and is hyperintense on T2-weighted images and hypointense on T1-weighted images. The lung parenchyma has intermediate signal intensity, which rises on T2-weighted images with increasing gestational age, and similarly decreases on T1-weighted images.
In cases of congenital diaphragmatic hernia, MRI can show herniation of the bowel loops and liver into the left hemithorax, with resultant hypoplasia of the left lung, Hayes noted. In another case of congenital cystic adenomatoid malformation, coronal MRI of a second-trimester fetus showed a large cystic malformation in the right hemithorax, with associated hydrops fetalis. Axial MRI of the thorax showed displacement of the heart, with a hypoplastic left lung.
In MRI, fast sequences are used to overcome image quality artifacts caused by fetal motion, and this can lead to the use of high specification magnetic field gradients; the frequency range for the gradients is from 1 to 10 kHz, according to Dr. Janet De Wilde, executive manager of SINAPSE (Scottish Imaging Network: A Platform for Scientific Excellence), University of Edinburgh, U.K. The main concerns are the clinical effects of low frequency EMF (electromagnetic field) induced currents and acoustic noise, but overall there is no evidence that the use of clinical MR procedures during pregnancy produces adverse effects.
She suggested avoiding scanning above the normal controlled limit, and if scanning in the first controlled level, then high specific absorption rate (SAR) sequences should be applied for as short a time as possible. High SAR sequences should be interspersed with low SAR sequences, and if the fetus or maternal abdomen are not the target organs of interest, then the fetus should be kept out of the transmit field of the RF coil, if possible.
Take care when scanning fetuses with poor placental function, for instance due to fetal growth restriction, added De Wilde. Maternal heat stress has been reported to reduce placental perfusion. Care should also be taken when scanning pregnant women with conditions leading to impaired thermoregulation, and pregnant women who are febrile should not undergo MRI. The mother's heat-loss pathways should be optimal, with no blankets, good bore air flow, and a reasonable room temperature, she said.
MRI is indicated for pregnant women if other nonionizing diagnostic imaging is inadequate, advises the Safety Committee of the Society of MRI. No adverse effects on fetal growth or development have been reported to date, although the biological effects of MRI are still uncertain during pregnancy, and the use of MRI should be limited in the second and third trimesters of pregnancy at an SAR of less than 3 W/kg. Gadolinium-based contrast media are not recommended because they cross the placenta and enter the fetal circulation within seconds after intravenous injection.