CHICAGO - CT is not needed in the vast majority of patients presenting with acute appendicitis, researchers in Spain have found. They presented their findings from a new study at the RSNA 2011 congress.
Ultrasound has high sensitivity and high positive predictive value for ruling out acute appendicitis, and it's useful for diagnosing several conditions that mimic the disease, avoiding additional tests in nearly all patients, according to radiologists from Hospital Universitario Severo in Madrid.
"Of those that had diagnostic imaging tests, 70% had only ultrasound, so it's very different from the U.S., said Dr. Javier Fernandez in an interview with AuntMinnieEurope.com. "And ultrasound has high sensitivity, a high positive predictive value, it's cheaper than CT, and it doesn't have radiation."
Acute appendicitis is the most frequent cause of acute abdomen in the emergency department and the most common indication for emergency abdominal surgery. Acute appendicitis remains a difficult diagnosis based on clinical examination and laboratory tests alone, with a negative laparotomy rate of 16% to 46% without imaging, Fernandez said. The use of imaging for diagnosing acute appendicitis has decreased the rate of negative laparotomies to 6% to 10%. Still, getting the diagnosis right -- and fast -- is important because the perforation rate is as high as 35% when surgery is delayed, he noted.
The study came about when surgeons asked the radiologists how they managed acute appendicitis, and how the decisions to image the patient and with which modality were made. The hospital didn't have a set diagnostic protocol and needed one.
The field is still evolving, Fernandez said. Researchers of a recent U.S. study found that the percentage of adult patients with appendicitis who were diagnosed by CT increased from 6% in 1996 to 69% in 2006 and from 0 to 60% in children.
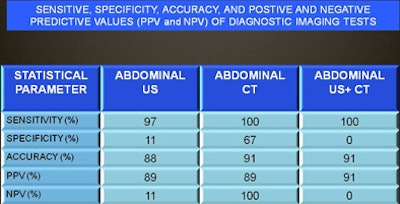
Fernandez said he was unaware of published studies analyzing the efficacy of different modalities in a similar setting. His group aimed to determine the accuracy of imaging tests, including ultrasound alone, CT alone, and CT plus ultrasound to diagnose acute appendicitis in the emergency department. The retrospective study included 165 consecutive patients who underwent emergency appendectomy for suspected appendicitis between January 1 and December 31, 2010. Data were gleaned from pathology and radiology reports, as well as from an administrative database.
Ultrasound was performed by a radiology resident with at least 12 months of training or staff with varying degrees of dedication to abdominal imaging. Patient demographic information, laboratory tests for C-reactive protein (CRP) and leukocytes, and pathology were reviewed.
The abdominal ultrasound group included patients who had been explored only with ultrasound. The CT group included those who had only CT (11 patients). The ultrasound plus CT group (n = 23) included patients whose ultrasound results were inconclusive and needed a CT as well. The most frequent reason for inconclusive ultrasound was not identifying the full length of the appendix or a certain section.
According to the results, 116 patients (70%) had imaging tests before the appendectomy, most frequently ultrasound (n = 82, 50%). Acute appendicitis was more common in men (n = 107, 67%). That means 30% went to laparoscopy without imaging, Fernandez said. The negative laparotomy rate was 3.6%, and the most common pathologic diagnosis was phlegmonous appendicitis in 60% of patients. All diagnostic imaging tests (ultrasound, CT, and ultrasound plus CT) had high sensitivity and high positive predictive values, he said.
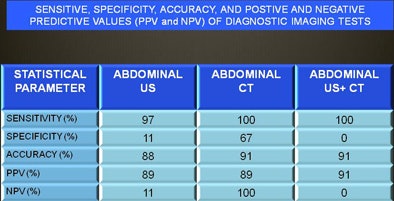 Results in 165 consecutive patients presenting to the emergency department with suspected acute appendicitis show comparable results for ultrasound, CT, and combined exams. Chart courtesy of Dr. Javier Fernandez.
Results in 165 consecutive patients presenting to the emergency department with suspected acute appendicitis show comparable results for ultrasound, CT, and combined exams. Chart courtesy of Dr. Javier Fernandez.At Hospital Universitario Severo, patients younger than age 5 or weighing less than 20 kg, with a clinical suspicion of appendicitis whether or not associated with an imaging test, are transferred to another facility, since the hospital does not have a pediatric surgery department, according to Fernandez. The study did not include patients with suspected clinical appendicitis and imaging tests in which surgery was not performed, and this is susceptible for further investigation, he noted.
Ultrasound is especially useful in young patients with either high CRP or leukocytosis. The modality is useful for ruling out appendicitis and diagnosing a wide range of conditions that mimic acute appendicitis, according to Fernandez.
"I think ultrasound should be the first test in managing appendicitis, and what I want to do in my hospital is propose a management protocol after the study this year," he said.
Ultrasound is also a good first choice for diagnosing acute abdomen, he added. In Spain, most ultrasound is done by radiographers, not by radiologists. Maybe the lack of skilled radiographers to perform ultrasound is one reason why CT is more common in the U.S., he suggested. In any case, he said, larger patients aren't necessarily a barrier to ultrasound. Even if the patient is much larger than the European norm, ultrasound can give the diagnosis if the organ is close to the surface, and it often is.
What about large studies in the U.S. concluding that CT has a higher sensitivity and lower rate of false positives than ultrasound in multicenter studies? In the U.S., ultrasound is less common and maybe not as successful. European countries have similarly high diagnostic rates for ultrasound, according to several studies, Fernandez noted. "I think we should always start with ultrasound," he said.