The rapid adoption of a new procedure for transcatheter aortic valve implantation (TAVI) reasserts a role for cardiac CT as an indispensible tool for anatomical assessment, preoperative planning, and postoperative evaluation.
TAVI was approved for use in Europe at the end of 2007, and by the end of 2009, more than 10,000 patients had received a prosthetic valve implanted by percutaneous coronary intervention. That number jumped to 40,000 just 18 months later, according to reports at the Paris Course for Revascularization (EuroPCR) from the manufacturers of the two devices holding a CE Mark approval.
Approval from the U.S. Food and Drug Administration (FDA) for the Sapien TAVI valve from Edwards Lifesciences is expected by the end of this year. The eligible U.S. patient population is estimated at more than 89,000 in 2012 and will exceed 103,000 by 2015, according to projections from analysts with Canaccord Financial and Wells Fargo Securities.
For characterization of native cardiac valves, examining suspected clinically significant valvular dysfunction and the characterization of prosthetic cardiac valves, cardiac CT can be valuable. A special session at EuroPCR 2011 reviewed the nuts and bolts of cardiac CT for TAVI with interactive case readings for coronary and structural heart disease to help interventional cardiologists acquire a systematic and practical approach to using this modality.
The learning curve will be steep for many, as a show of hands prompted by session co-chairman Dr. Jeroen Bax, PhD, from the Leiden University Medical Center in the Netherlands, revealed fewer than about a quarter of the participants were currently using CT in routine practice.
"There is an increasing use of CT, and I believe one of the new indications to be addressed in the 2012 guidelines will be for valvular disease before the procedure," said session co-chair Dr. Filippo Cavia from the Cardiac Thoracic Centre in Monaco. "With all the new imaging modalities, we are pushing a kind of revolution in patient management."
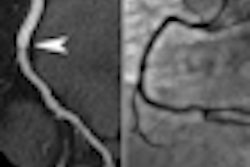
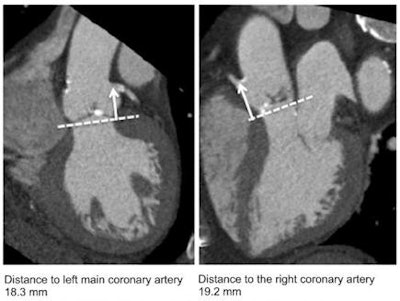
Bax's colleague from the Leiden center, Dr. Victoria Delgado, PhD, described in detail the critical role cardiac CT plays in the planning and follow-up of TAVI patients. In a first step, cardiac CT can confirm the severity of aortic stenosis and also is essential for determining the feasibility of the procedure with measurement of the aortic valve dimensions and aortic root anatomy. The maximum and minimum annular dimensions are key to the selection of the appropriate valve replacement, and the distance to the coronary ostia is critical in procedural success and the eventual need for a pacemaker after placement of the prosthesis.
Cardiac CT measurement of aortic root anatomy
 Images provided by Dr. Victoria Delgado, PhD, Leiden University Medical Center, the Netherlands, from her presentation "CT for Coronary and Structural Heart Disease" at EuroPCR 2011.
Images provided by Dr. Victoria Delgado, PhD, Leiden University Medical Center, the Netherlands, from her presentation "CT for Coronary and Structural Heart Disease" at EuroPCR 2011.A transfemoral approach for percutaneous delivery of the valve is the preferred route with an 18-French device and the coronal, sagittal, and axial views of the peripheral arteries help plan the alignment of the catheter centerline along the entire vessel. For patients that CT reveals have tortuous or blocked peripheral arteries, an alternative implantation through a carotid artery or between the ribs with a 24-French valve needs to be planned.
Finally, CT is uniquely suited for follow-up evaluation of the prosthesis position and deployment, as well as detection of complications, such as valvular leaks.
"Echography can be a problem after implantation of a stented device like a valve, and here multislice CT becomes key for showing the results of the procedure," Delgado said.
The rich clinical information revealed by cardiac CT has led to an overuse of these exams and provoked wide discussion and debate. Six months ago, the publication of the Appropriate Use Criteria for Cardiac CT (Journal of the American College of Cardiology, November 23, 2010, Vol. 56:22, pp. 1864-1894) -- drafted jointly by eight professional societies -- brought a much-needed update to guidance, satisfying the concerns of payers over runaway costs and patient groups for unnecessary exposure to radiation.