Fresh guidelines from the European Society of Urogenital Radiology (ESUR) on dealing with uterine cervical cancer patients have added weight to the value of MRI as the imaging modality of choice for preoperative staging and follow-up.
Most cervical cancers are diagnosed at an advanced stage, and thus are not suitable for surgical staging, according to researchers writing in the May edition of European Radiology. Cervical cancer remains a clinically staged disease, but there are significant inaccuracies in the clinical staging system compared with surgical staging. Physicians struggle the most with accurate estimation of tumor size, the assessment of parametrial and pelvic side wall invasion, and the evaluation of lymph node metastases, which are recognized important prognostic factors.
In 2009, the International Federation of Gynecology and Obstetrics (FIGO) encouraged for the first time the use of imaging techniques for staging. To that end, the female pelvis subcommittee of ESUR formed a working group to establish technical guidelines for uterine cervical cancer staging with MRI based on clinical practice.
All 11 ESUR members recommended MRI for staging tumors classified as 1B1 or smaller tumors if trachelectomy is being considered. They all also recommended MRI for treatment follow-up and detecting tumor recurrence (Eur Radiol, May 2011, Vol. 21:5, pp. 1102-1110).
Regarding MRI time delay after follow-up, the members' recommendations varied from three weeks to six months, with the majority recommending three to six months after completion of
chemoradiation therapy and brachytherapy. Regarding patient follow-up, some ESUR members perform yearly follow-up MRI for five years, and some only if there are symptoms of recurrence.
 Dr. Corinne Balleyguier from the radiology department at Institut Gustave Roussy in Villejuif, France.
Dr. Corinne Balleyguier from the radiology department at Institut Gustave Roussy in Villejuif, France.
When it comes to imaging the patient, high-field MRI should include at least two T2-weighted sequences in sagittal, axial oblique, or coronal oblique orientation of the pelvic content, according to lead author Dr. Corinne Balleyguier from the radiology department at Institut Gustave Roussy in Villejuif, France.
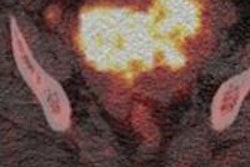
The axial T1-weighted sequence is useful to detect suspicious pelvic and abdominal lymph nodes, and images from symphysis to the left renal vein are required, the researchers also found. The intravenous administration of gadolinium contrast is optional but is often required for small lesions (< 2 cm) and for follow-up after treatment, they wrote.
Diffusion-weighted sequences are optional but recommended to help evaluate lymph nodes and detect a residual lesion after chemoradiotherapy, they added.
"I don't know what impact it will have but these guidelines are just rules of good practice," Balleyguier wrote in an email to AuntMinnieEurope.com.