Advanced MDCT scanning may be ready to play an important role in assessing noncalcified coronary artery plaque, say German researchers, who used a 256-detector-row scanner and plaque-volume measurement software to compare interobserver variability in patients with different types of plaque.
The researchers found that interobserver variability was high when expert readers measured the volume of mixed and calcified plaques, but there was far less variability when measuring noncalcified plaque volume (International Journal of Cardiovascular Imaging, August 2010, Vol. 26:6, pp. 711-720).
Unfortunately, there are no standards for identifying and quantifying so-called "soft" coronary artery plaques, as there are for calcified lesions, noted Oliver Klass, MD, and colleagues from the University of Ulm in Germany.
The association between calcified coronary artery plaque and myocardial infarction is well established, but retrospective studies have also shown an association between plaques containing noncalcified components and presentation with acute coronary syndrome. The association between soft plaque and adverse events could be better defined if standards for measuring it were developed, the authors noted.
Their study aimed to evaluate the potential clinical value of coronary plaque imaging with a new-generation CT scanner, measuring the interobserver variability of coronary plaque assessment with a new semiautomatic plaque analysis application.
The researchers looked at 35 isolated plaques of the left anterior descending coronary artery in 35 patients (mean age, 58 ± 11 years; range, 38-80) with the new semiautomatic plaque analysis application. Only isolated plaques were selected in an effort to simplify validation of automated plaque volumes.
All patients were scanned using a 256-detector-row Brilliance iCT scanner (Philips Healthcare, Andover, MA) following administration of iodinated contrast and saline.
Prospectively triggered images were acquired at 256 x 0.625 mm, 120-140 kVp, 150-250 mAs, and a 2 x 128 x 0.625-mm collimation with dynamic z-focal spot and a z-increment of 62.4 mm between axial acquisitions. X-rays were triggered at 75% of the RR interval and included a "buffer" of 90 msec of tube time to ensure adequate coverage. The effective tube current-time product was 600 to 1,000 mAs, depending on body weight.
The images were reconstructed at a thickness of 0.9 mm and an increment of 0.45 mm using an enhanced semismooth reconstruction kernel (XCB). Two independent readers examined lesion volume, maximum plaque burden, lesion attenuation, and mean and standard deviation, as well as relative lesion composition on a dedicated cardiac workstation (Cardiac Viewer and Comprehensive Cardiac Analysis, Brilliance Workspace, Philips Healthcare) that was integrated with the plaque analysis software.
In all, CT found 10 noncalcified, 16 mixed, and nine calcified lesions in the study cohort. "Relative interobserver bias and variability for lesion volume were -37%, -13%, -49%, -44% and 28%, 16%, 37%, and 90% for all, noncalcified, mixed, and calcified lesions, respectively," the authors wrote.
While mixed and calcified lesions showed a high degree of lesion volume interobserver variability, noncalcified lesions had less interobserver variability in lesion volume. "Absolute interobserver bias and variability for relative lesion composition were 1.2%, 0.5%, 1.5%, 1.3% and 3.3%, 4.5%, 7.0%, and 4.4% for all, noncalcified, mixed, and calcified lesions, respectively," they wrote.
|
||||||||||||
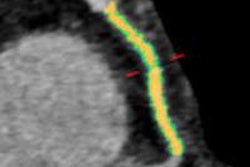
| Interobserver variability was lowest for noncalcified plaque. All data reported as mean ± standard deviation [minimum-maximum]. |
"In contrast to the mixed and calcified lesions, the interobserver variability in lesion volume and maximum plaque burden for the 10 noncalcified lesions (≤ 10% calcified content) was much lower," the authors wrote. With a cumulative interobserver variability for noncalcified lesions of less than 28.5%, the current study's results are better than or comparable to other studies of MDCT-based plaque assessment, they added.
"Since interobserver variability is often the major contributor to decreased measurement reproducibility, it is also a primary limitation for longitudinal assessment," Klass and his colleagues wrote. "Therefore, the interobserver variability is the lower bound with which lesion volume differences can be measured over time. In this way, the minimum amount of plaque regression or progression that may be detected, despite interobserver variability, for noncalcified lesions would be greater than 28.5%."
The higher interobserver variability associated with quantifying calcified lesions seems to be of limited clinical value considering the existence of well-validated and readily available software applications for quantifying coronary calcium, they noted.
As for the study's limitations, selection bias was present, as patients with only a single isolated left-anterior-descending artery lesion were included, and total plaque burden was not assessed for each patient. In addition, the study had a relatively small sample size, and automated MDCT-derived volumetric lesion parameters were not compared to a reference standard such as intravascular ultrasound.
The low interobserver variability in noncalcified lesions means "there may [be] a role for MDCT in serial noncalcified plaque assessment with semiautomatic analysis software," they wrote.
By Eric Barnes
AuntMinnie.com staff writer
September 8, 2010
Related Reading
SHAPE II task force revising cardiac risk guidelines, August 17, 2010
Coronary calcium usually ignored on chest CT, August 12, 2010
Ultrasound finds high heart disease risk in some low-risk women, July 7, 2010
Coronary calcium score doesn't help predict risk in low-risk men, June 7, 2010
CT equivalent to IVUS for culprit plaque detection, December 4, 2008
Copyright © 2010 AuntMinnie.com