Computer-aided detection (CAD) software yields a higher level of sensitivity for identifying lung nodules as a second reader than when used concurrently during image interpretation, according to research from the University of Verona in Italy.
In a retrospective review, the research team found that applying CAD as a second reader after an initial reading session by a radiologist led to a higher level of sensitivity than either using CAD as a concurrent reader or reading without CAD. The advantages of CAD as a second reader came with the cost of significantly longer reading time, however.
Although CAD has been shown to boost radiologist sensitivity for detecting pulmonary nodules, the issue of which method of CAD use provides the best results has remained unclear, according to Dr. Giovanni Foti, who presented the research during a scientific session at the 2010 European Congress of Radiology (ECR).
Foti and colleagues sought to compare the sensitivity and reading time obtained using CAD software as a second reader and as a concurrent reader in a retrospective review of 125 consecutive oncologic patients undergoing nonenhanced chest CT studies.
Twenty-five patients were excluded from the study due to poor collaboration, pleural effusion, pneumonitis, or previous lung surgery, according to Foti. The remaining 100 patients included 52 males and 48 females.
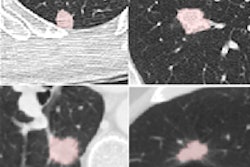
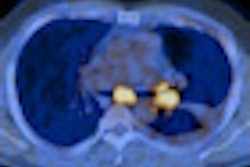
Images were generated on a Brilliance CT 64-slice scanner (Philips Healthcare, Andover, MA) using parameters of 1-mm slice thickness, 120 kV, 200 mAs, and a 300-mm field-of-view. Images were visualized on a dedicated workstation using maximum intensity projection (MIP) reconstruction based on the reader's preference.
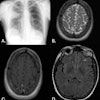
Two board-certified radiologists and two residents participated in the study. All readers were asked to identify all of the solid lung nodules between 3 and 30 mm in diameter, Foti said. Calcified nodules and ground-glass opacities were excluded. A fifth radiologist created the reference standard by comparing the findings of the four radiologists to obtain consensus.
The two board-certified radiologists (readers 1 and 2) first read the studies without CAD, and then, at least two months later, interpreted the studies with the use of CAD as a second reader. In the third phase of the study, the two residents (readers 3 and 4) interpreted the studies using CAD as a concurrent reader.
Consensus reading determined that there were 258 nodules 3 mm and larger, including 224 nodules 5 mm and larger.
Reader sensitivity for all lung nodules
|
The increased sensitivity from the use of CAD as a second reader (readers 1 and 2) was statistically significant compared to reading without CAD (p < 0.001) and with the use of CAD as a concurrent reader by readers 3 and 4 (p < 0.025). However, when readers 3 and 4 used CAD as a concurrent reader, they did not have a statistically significant increase in sensitivity compared to readers 1 and 2 reading without CAD (p > 0.05).
The CAD software produced a mean of four false-positive findings per study, Foti said. However, readers 1 and 2 experienced a reduction in false-positive findings from the use of CAD.
CAD turned in standalone sensitivity of 62.8% at the 3-mm nodule threshold and 67.4% at the 5-mm threshold, Foti said.
In other findings, the use of CAD as a second reader took a mean of 330 seconds, significantly higher than the mean of 135 seconds for reading without CAD (p < 0.001) and the mean of 195 seconds with CAD as a concurrent reader (p < 0.025).
"The use of software as concurrent reader [readers 3 and 4], without a significant increase in reading time, does not allow a significant increase in sensitivity in identifying pulmonary nodules compared to when reading without the software," Foti concluded. "The use of CAD software as a second reader, at the cost of longer reading time, increased sensitivity if compared to reading without the software or using the software as a concurrent reader."
By Erik L. Ridley
AuntMinnie.com staff writer
May 7, 2010
Related Reading
Lung CAD boosts radiologist accuracy, February 17, 2010
Integrating CAD with PACS adds clinical value, December 18, 2009
CT lung CAD helps readers differently, November 4, 2009
Brazilian team marries lung CAD with PACS, August 20, 2009
CARS report: New CAD tool follows lung nodules over time, June 30, 2009
Copyright © 2010 AuntMinnie.com